Have you been diagnosed with a varicocele? Are you exploring treatment options, especially if you’re dealing with infertility or chronic testicular pain? This Tower Urology article will explain the benefits and drawbacks of microsurgical varicocelectomy and varicocele embolization for clinical varicocele.
Both procedures aim to correct abnormal blood flow in the testicular veins and are usually done on an outpatient basis. However, they differ significantly in technique, effectiveness, and recovery. Here’s a straightforward overview to help you choose the best option for you.

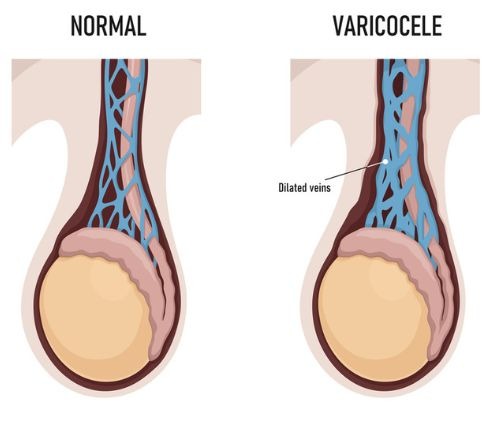
Let’s be clear: what is a varicocele?
The scrotum is a loose bag of skin that holds your testicles. Like other body parts, the scrotal sack contains veins. These veins are part of your spermatic cord. Their job is to carry blood away from your testicles after oxygen has been delivered.
Sometimes, the valves in these veins don’t work properly, causing blood to stay in the veins instead of flowing normally. As a result, the veins enlarge, like varicose veins in your legs. This condition is called a varicocele. Most likely, your varicocele started during puberty and developed gradually.
Usually, varicoceles develop on the left side. Left varicoceles are caused by the male anatomy. On your left side, your internal spermatic vein joins your left renal vein at a sharp angle, which reduces smooth blood flow.
On your right side, your spermatic vein drains into the much larger inferior vena cava, so blood flow is less restricted. Sometimes, there is a varicocele in both testicles, known as a bilateral varicocele. Many varicoceles go unnoticed. If you are aware of yours, it’s likely because either it causes discomfort or pain, or a semen analysis has shown suboptimal sperm parameters related to fertility.
Andrology, the science and medicine focused on male health, especially male reproductive functions, has made significant progress in detecting and treating varicoceles. However, there is still more to learn.
Microsurgical Varicocelectomy
Microsurgical varicocelectomy is a precise laparoscopic surgical procedure. This surgical approach is carried out under high-powered magnification. Through a small incision in the groin or lower abdomen, the surgeon identifies and ligates (ties or closes off) the abnormal veins while carefully preserving arteries and lymphatics.
Advantages:
- Highest success rates: Success rates exceed 98% when performed by experienced microsurgeons.
- Lowest recurrence rates: Less than 1%, significantly lower than other methods.
- Most effective for improving fertility: Studies consistently show improvement in semen parameters such as sperm count and motility (movement). Thus, pregnancy rates increase after this surgical treatment.
- Superior pain relief: Particularly effective for men suffering from chronic testicular pain caused by varicoceles.
- Minimized complications: Microsurgery allows for precise identification and preservation of key structures, including the testicular artery, reducing the risk of hydroceles and testicular atrophy.
Considerations:
- Requires general or regional anesthesia
- Surgical recovery: Most men return to normal activity within 1–2 weeks.
- Slight risk of complications: As with any surgery, there is a minor risk of infection, swelling, or hematoma.
Varicocele Embolization
An “embolization” is a “blocking.” In this case, blocking the problematic vein prevents blood from entering it. This type of varicocele repair is called a varicocele embolization. It is a non-surgical, minimally invasive procedure performed by an interventional radiologist.
The first step in this embolisation procedure is to insert a catheter into a vein (usually in the groin or neck). Then, through this catheter, your interventional radiologist will either insert tiny metal coils, which block the blood flow, or a liquid sclerosant, which will cause the problematic vein to shrink.
Advantages:
- Minimally invasive: No incision; performed through a vein using imaging guidance.
- Local anesthesia only: Ideal for patients who want to avoid general anesthesia.
- Quick recovery: Most men resume regular activities within a few days.
- Alternative option: Useful for patients who’ve had prior groin surgery or who are not candidates for surgery.
Considerations:
- Higher recurrence and failure rates: Recurrence can range from 10–20%, depending on technique and anatomy.
- Less reliable for pain: Embolization tends to be less effective for men with varicocele-related pain.
- Variable fertility outcomes: While postoperative sperm parameters may improve, reducing male infertility, microsurgical repair tends to deliver more consistent fertility results.
- Radiation exposure: Involves fluoroscopy (X-ray), although exposure is minimal.
Side-by-Side Comparison
Check out this quick view of the differences between these two treatments of varicoceles.
| Varicocele Embolization | Microsurgical Varicocelectomy | Feature |
| ~80–90% | 98-99% | Success Rate |
| 10–20% | Less than 1% | Recurrence Rate |
| Variable results | Strong evidence of improvement | Fertility Impact |
| Less predictable | High success | Pain Relief |
| Local only | General or regional | Anesthesia Required |
| 2–5 days | 1–2 weeks | Recovery Time |
| No incision (through a vein) | Surgical incision | Invasiveness |
| Minimal | None | Radiation Exposure |
Which Option Is Best for You?
- For men with infertility or chronic testicular pain, microsurgical varicocelectomy is typically the preferred option because of its precision, lower recurrence rate, and consistent outcomes.
- For men seeking a less invasive option or who are not candidates for surgery, varicocele embolization can be a suitable alternative, especially when performed at a center with extensive interventional radiology experience.
Why Tower Urology is your best choice for varicocele treatment in Los Angeles
At Tower Urology, our multidisciplinary team includes fellowship-trained microsurgeons who will address your varicocele concerns, whether they involve testicular pain or fertility issues. This allows us to customize varicocele treatment based on your goals, anatomy, fertility plans, and overall health.
We invite you to establish care with Tower Urology.
Tower Urology proudly affiliates with Cedars-Sinai Medical Center, ranked #1 in California and #2 nationwide by U.S. News & World Report. This partnership demonstrates our commitment to providing the highest quality urologic care alongside top urologists in Los Angeles. Our extensive experience and access to Cedars-Sinai’s world-class facilities ensure that our exceptional and innovative urological services position Tower Urology as a leader in Southern California.
Tower Urology is easily accessible for patients across Southern California and Los Angeles, including Beverly Hills, Santa Monica, West Los Angeles, West Hollywood, Culver City, Hollywood, Venice, Marina del Rey, Burbank, Glendale, and Downtown Los Angeles.
Our services include treatment for low testosterone, chronic pelvic pain, chronic testicular pain, and Peyronie’s disease.
Sources
Percutaneous Treatment of Varicocele with Microcoil Embolization: Comparison of Treatment Outcome with Laparoscopic Varicocelectomy
https://journals.sagepub.com/doi/10.2310/6670.2009.00062
Efficacy of varicocele embolization versus ligation of the left internal spermatic vein for improvement of sperm quality
https://www.jvir.org/article/S1051-0443(22)00126-9/abstract
Comparing Endovascular and Surgical Treatments for Varicocele: A Systematic Review and Meta-Analysis
https://www.jvir.org/article/S1051-0443(22)00126-9/abstract