The recent announcement of President Joe Biden’s diagnosis with metastatic prostate cancer has sparked a wave of concern and confusion. How could a leader of the most technologically advanced nation in the world receive such a late-stage diagnosis? This situation highlights flaws in our current screening guidelines and offers a moment to revisit how we approach prostate cancer detection, especially in aging men.
Understanding Prostate Cancer and Screening

Prostate cancer is the abnormal growth of cells in the prostate gland. It can spread and invade other tissues, often without producing any symptoms. Most patients—like President Biden—are asymptomatic at diagnosis. In many cases, the only reason prostate cancer is detected is due to a digital rectal examination (DRE) or a blood test measuring prostate-specific antigen (PSA).
PSA testing, introduced in the 1980s, measures the level of prostate-specific antigen in the blood. Elevated levels can indicate cancer but can also result from benign conditions like infection or prostate enlargement. Interpretation must be age-specific and consider prostate gland size, among other factors. When PSA or DRE results are abnormal, modern imaging tools like prostate MRI can provide additional insight.
Risk Factors
Several well-established risk factors increase the likelihood of developing prostate cancer:
- Age: The most significant risk factor.
- Race: African American men are more likely to develop aggressive forms of the disease.
- Genetics: A family history, especially in first-degree relatives, increases risk.
- Diet: A Western diet high in saturated animal fats has been linked to a higher incidence.
Contrary to some beliefs, chronic inflammation, smoking, alcohol, and benign prostate growth are not considered significant risk factors.
The Scope of the Disease
Prostate cancer is the most commonly diagnosed cancer in men. Annually:
- Around 300,000 men are diagnosed.
- Approximately 50,000 die from the disease.
- About 3 million men live with prostate cancer in the U.S.
Despite its prevalence and mortality rate—exceeding that of pancreatic, liver, bladder, esophageal cancers, and lymphomas—screening remains a controversial issue.
The Screening Debate: A History of Mixed Messages
Medical organizations have long debated the merits of PSA screening. The U.S. Preventive Services Task Force (USPSTF), in particular, has shifted its stance multiple times:
- 2002: Declared insufficient evidence to recommend for or against screening.
- 2008: Advised against screening men over 75, stating harms outweighed benefits.
- 2012: Issued a blanket recommendation against PSA screening, regardless of age (Grade D). Notably, the panel did not include any urologists or prostate cancer specialists.
The core issue is not screening itself, but the potential for overdiagnosis and overtreatment. Nevertheless, the 2012 recommendation had measurable consequences. For the first time in decades, prostate cancer mortality began to rise, coinciding with fewer early-stage diagnoses and more men presenting with advanced disease.
The implications of President Biden’s Diagnosis
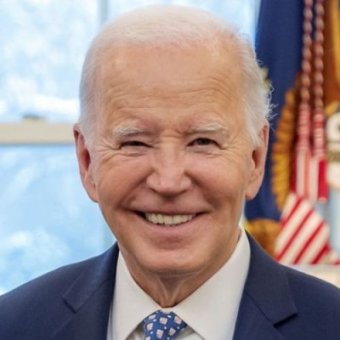
If President Biden was not receiving routine PSA tests or DREs, his diagnosis of metastatic prostate cancer suggests a troubling failure in prevention. The USPSTF’s flawed, one-size-fits-all approach may bear some responsibility. Older men, though at higher risk of dying from other causes, are also more likely to develop aggressive prostate cancer and less likely to survive once diagnosed at a late stage
Medical advancements are extending life expectancy; about 25% of men in their 70s will live to age 90 or beyond. As longevity increases, the logic behind limiting screening for older adults becomes less defensible.
A Call for Individualized Care
The takeaway from this national conversation should not be to abandon PSA testing, but to refine our approach. Screening recommendations must be individualized, especially for healthy older men who may benefit significantly from early detection.
The USPSTF’s current recommendations ignore this nuance. We must recognize that metastatic prostate cancer is common—and deadly—in men over 70. With personalized screening strategies, we can catch it earlier, treat it more effectively, and save lives.
Have questions or concerns about your prostate health? Tower Urology is here for you in Los Angeles.
Our board-certified, fellowship-trained urologists are here. We will help address any concerns you may have and support you on your health journey. Feel free to reach out to the physicians at Tower Men’s Health at (855) 246-2700.