Loss of bladder control (urinary incontinence) after prostate surgery is a devastating complication, which has a significant negative impact on quality of life. The ‘good news’ is that with appropriate evaluation and treatment, the incontinence problem is usually treatable with substantial improvement in quality of life.
It is not unusual that lack of bladder control is a problem for the first few months following radical prostatectomy. A biofeedback program may be helpful during this period to help restore bladder control. When urinary incontinence persists more than 3-6 months after radical prostatectomy, appropriate bladder testing, called urodynamics, is critical to evaluate the function of the bladder and sphincter (valve) muscle to determine the exact cause of the post-prostatectomy incontinence (PPI).
Urodynamic testing is performed in the office and typically takes approximately 20 minutes to complete. The test involves filling the bladder through a special catheter inserted in the penis while measuring the pressures in the bladder. During the test, various maneuvers are performed to evaluate the bladder function, demonstrate the urinary incontinence, and thus specifically define the cause of the urine loss.

Normally, as the bladder fills, there is very little change in bladder pressure, and the sphincter remains closed, allowing the man to stay dry. When incontinence occurs following prostatectomy, this normal balance of bladder and sphincter function is disturbed.
Our research has defined three main causes of PPI based upon urodynamic findings:
1. High pressure (with ‘spasms’ of the bladder) developing in the bladder as the bladder fills (50% of men with PPI). These bladder spasms may be related to nerve damage that may occur as a result of the prostatectomy. These bladder spasms may cause urge incontinence (the need to rush to get to the bathroom), frequent urination, and sometimes loss of urine at night. This high-pressure bladder dysfunction can also occur following pelvic radiation therapy. Normally, when the bladder fills, the pressure remains low, even with any spasms.
2. Damage to the sphincter muscle (35% of men with PPI). This damage results in stress incontinence, characterized by the loss of urine during changes in position, coughing, straining, or vigorous physical activity.
3. A combination of bladder spasms and sphincter damage (10% of men with PPI). Men with this combined problem usually experience “mixed incontinence” symptoms with a combination of both urge and stress incontinence.
Treatment Options
Biofeedback/ Pelvic Floor Training may be a treatment choice in men who are incontinent and desire treatment early after radical prostatectomy (especially within the first 3-6 months following surgery). Biofeedback is also a useful treatment option in men who have more minor degrees of incontinence. The treatment program consists of weekly one-hour sessions with a trained therapist. A special sensor is inserted into the rectum and attached to the biofeedback computer. During the treatment session, the patient is taught to contract and strengthen the pelvic muscles, with the resulting muscular contraction displayed on the computer screen.
Additionally, an electrical signal can be sent to these pelvic muscles to help strengthen them. Each week, the goal is to strengthen the muscles. Many men experience significant improvement in bladder control with this biofeedback program.
When the main cause of the incontinence is high bladder pressures, medications to relax the bladder are usually effective. These medicines work by blocking nerve receptors in the bladder. Blocking these receptors results in decreased bladder contractility and improvement in bladder spasms. Medicines to relax the bladder (generally known as anticholinergics) include Enablex, Vesicare, Ditropan XL, Detrol LA, the oxytrol patch, oxybutynin 3% gel, and imipramine.
Side effects of these medications may include dry mouth, constipation, and blurry vision. These drugs should not be used in patients with uncontrolled narrow-angle glaucoma or in men who do not empty their bladders well. There is also a new type of oral medication, called Myrbetriq, that helps relax the bladder by stimulating different receptors in the bladder wall. Thus, Myrbetriq does not cause the typical dry mouth and constipation side effects commonly associated with other medications that have been used for years.
However, 10% of those who take Mybetriq may experience some increase in blood pressure. Many men who have not been able to tolerate the traditional medications used in the past benefit from this new medication.
When the oral medications fail to control the high bladder pressures, the Interstim “bladder pacemaker” device can be an excellent treatment option. This bladder pacemaker device can be tested in the office, with 70% of the patients responding promptly during the seven-day test. If there is a beneficial response to the seven-day test, implantation of the permanent bladder pacemaker can be considered. This procedure is performed as an outpatient under local anesthesia.
Another option for controlling high bladder pressures when the oral medications are not successful is Botox injection into the bladder. Botox is injected in an office setting through a cystoscope, with a success rate of approximately 50%.
Botox typically has a maximum duration of benefit of around six months, requiring regular repeat injections to maintain its effects. There is also a 5% risk of urinary retention associated with Botox injection. Should urinary retention occur, the patient may be required to perform self-catheterization 3 to 4 times per day until the effect of the Botox diminishes. Medicare now covers both the Interstim bladder pacemaker device and Botox injection.
Options for treatment of sphincter damage include biofeedback, injection therapy (which is generally not successful), the artificial urinary sphincter, and the male sling procedure. Those men with “mixed” bladder and sphincter malfunction undergo initial treatment (usually with anticholinergic drugs, Interstim, or Botox) to improve their bladder function (i.e., lower their bladder pressures), followed by treatment to address the weak sphincter (if necessary). Commonly, follow-up urodynamic studies are performed to evaluate the response to each stage of therapy.
Interstim “Bladder Pacemaker”
When the usual medical treatments to lower high bladder pressures are not successful, the Interstim “bladder pacemaker” may be an excellent alternative. This treatment involves an office test with placement of wires next to the nerves that control the bladder with local anesthesia. For seven days, the patient wears a battery-powered belt that sends an electrical signal to the nerves controlling the bladder, causing the bladder to relax.
The office test of the Interstim device has an approximately 70% success rate. The patient responds well to the office test; the permanent Interstim device is implanted as an outpatient procedure in the hospital under local anesthesia. This procedure involves placing a special stimulation electrode in the lower back next to the main nerve that controls the bladder (Figure 1a). This stimulation electrode is placed through a special needle under local anesthesia without the need for a large incision.
Next, the implantation of an internal ‘pacemaker’ generator that is attached to the stimulation electrode is performed and programmed through the skin (Figure 1b). The generator is very similar to a heart pacemaker, featuring a battery that typically lasts 8 to 10 years.
Overall, approximately 70% of patients respond to the office trial of test stimulation. When we proceed with the permanent implant, approximately 85% of patients have an excellent response. Use of the Interstim “bladder pacemaker” is an effective, relatively “non-invasive” treatment option for those patients who have high-pressure bladder dysfunction who do not respond to the usual forms of medical treatment.
Surgical treatments of stress incontinence due to sphincter damage following prostatectomy include the Artificial Urinary Sphincter (AUS) and the Male Sling Procedure. In general, injection therapy (i.e., collagen, Durasphere, etc.) has not been successful in men with sphincter weakness. This lack of success is due to the migration of the injected material away from the sphincter area after injection.
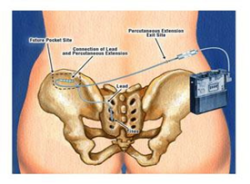
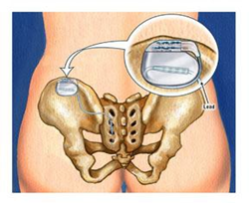
Figure 1a: Interstim stimulation electrode placed next to the nerve that controls the bladder.
Figure 1b: Internal Interstim generator attached to stimulation electrode.
The Artificial Urinary Sphincter (AUS)
Perfected over the last 30 years, the artificial urinary sphincter is a device implanted into the body to correct stress incontinence in men with significant sphincter damage. The AUS has three components: a cuff that helps close the urethra, a pump placed inside the scrotum, and a pressure-regulating balloon that is placed in the lower abdomen (see Figure 2). When the man wants to urinate, he squeezes the pump in the scrotum, which opens the cuff around the urethra. Automatically, after 3-5 minutes, the fluid returns to the cuff, allowing it to close. After the device is tested during surgery, the cuff is “locked” open and is only activated when swelling around the pump is gone (usually about 4-6 weeks after surgery).
With the current model of the AUS, long-term patient satisfaction has been excellent, with a mechanical malfunction rate of less than 15% at 10 years after device implantation. Despite these excellent long-term results, however, some men are hesitant to have this prosthetic device placed. For these men, as well as for those with more minor degrees of ppi (or for men who do not have the manual dexterity to squeeze the pump in the scrotum), the male sling is a promising alternative.
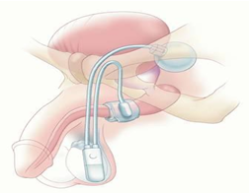
Figure 2: Artificial Urinary Sphincter in place.
Male Sling Procedure
Over the last few years, the male sling procedure has become a viable treatment alternative for men with ppi due to sphincter damage causing stress incontinence. The “best” candidates for the male sling are men with more minor degrees of stress incontinence (< 2 pads/day), men with no previous history of pelvic radiation therapy, and men who have not had a previous AUS inserted. The surgical procedure to implant the sling takes about one hour and can be done either on an outpatient basis or with an overnight hospital stay. The purpose of the “sling” is to compress the urethra and help eliminate loss of urine with coughing, sneezing, or vigorous activity.
The sling is placed via an incision between the scrotum and rectum (see figure 3). In the author’s experience, the most effective material used for the sling is a specially prepared synthetic patch that compresses the urethra. A catheter is usually left in place for 24 hours with most men being able to urinate with good control immediately after the catheter is removed.
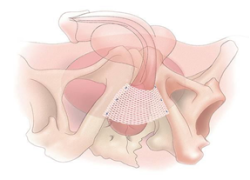
Figure 3: Male sling secured into position.
Thus far, the results with the male sling in properly selected patients have been encouraging. Approximately 30% of men are completely dry, 40% are significantly improved, and 30% are considered failures. Should the male sling not be effective, an artificial urinary sphincter may be regarded as a second alternative.
Summary
Recent advances in the evaluation and treatment of men with incontinence following prostate surgery have allowed many men to regain their urinary control and improve their quality of life. Men with significant incontinence following treatment for prostate cancer should have an appropriate evaluation (i.e., urodynamic testing) to determine the exact cause of their incontinence. Appropriate treatment based on the results of this testing usually results in a significant restoration of bladder control and an improved quality of life.
Sources:
1. G Leach, B Trockman, and A Wong, et al.: Post-prostatectomy incontinence: urodynamic findings and treatment outcomes. J. Urology 155:1256,1996.
2. F Haab, B Trockman, P Zimmern, and G Leach: Quality of life and continence assessment of the artificial urinary sphincter in men with minimum 3.5 years of follow-up. J. Urology 158:435-439,1997.