What is a prostate biopsy?
A referral for a prostate biopsy — a diagnostic procedure to extract small tissue samples from the prostate gland — is often received with trepidation and anxiety.
But for patients who’ve had an alarming blood test result or are worried about a suspicious scrotum lesion, it’s best not to delay the biopsy date. Fortunately, medical technology offers us better, less invasive, and more accurate ways to resolve the issue.

How is a prostate biopsy performed?
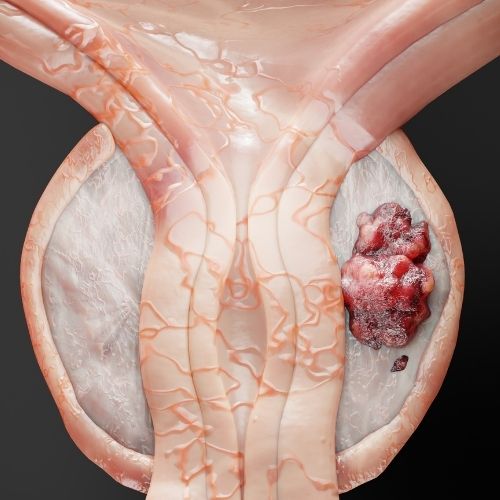
A man’s prostate gland is a walnut-shaped organ responsible for producing semen. It’s located between the bladder, the rectum, and the urethra, which means it’s not easily accessible.
Regardless of the technique used, all prostate biopsies have the same fundamental goal: to enter the prostate gland with a very fine needle, extract a small piece of prostate tissue, and check this sample carefully for cancer cells.
A positive biopsy can also tell us what type of cancer it is, how quickly it’s likely to grow, and which medications it may respond best to.
What are the different types of prostate biopsies?
Nowadays, urologists classify biopsies into two main types.
Ultrasound-guided transrectal biopsy (TRUS)
TRUS involves passing the biopsy needle through the wall of the rectum, usually guided by ultrasound, to reach the right spot. This is easier to do with local anesthesia and sedation. However, entering through the back this way makes it harder to get to the front of the prostate, so results may not be as accurate and may fail to find the tumor, resulting in a false negative.
This ultrasound method also carries a higher risk of infection, especially in the urinary tract, as bacteria from the colon can be pushed into other organs by the needle or the probe.
Transperineal biopsy
This technique starts with a small cut in the perineum (the soft area right in front of the anus). We then use this hole to insert a needle and an ultrasound probe.
From this side, it’s generally easier to reach all areas of the prostate, which allows your urologist to do a prostate mapping and take small samples across the prostate, providing more accurate results.
Steering clear of the rectum also carries a much lower risk of infection.
While superior to a TRUS procedure, a transperineal prostate biopsy is also more painful. It may require general anesthesia or heavy sedation, which means it cannot be carried out in a regular office, and the patient will likely need to be admitted to a hospital for a day.
What is a UroNav fusion biopsy system?
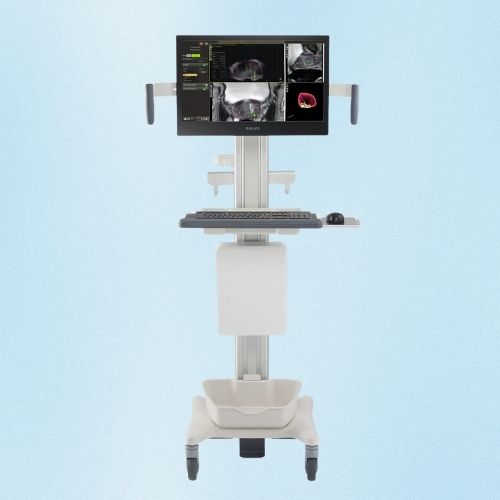
The UroNav fusion biopsy system is a newer method that combines the accuracy and safety of a transperineal biopsy with the relative ease of a TRUS procedure. Although it’s only been around for the last decade, researchers already recognize UroNav as more accurate than a standard transrectal biopsy, and it’s poised to become the new standard in prostate care.
The UroNav system combines MRI images taken a few days or weeks before the biopsy with live ultrasound images. It uses a tiny tracking sensor attached to the transrectal ultrasound probe, which allows us to track the device’s location and orientation on a computer screen.
The information from the sensor and the sound waves of the ultrasound probe, combined with the map created by the MRI images, enables us to guide the needle with remarkable accuracy. This means healthcare providers can:
- Target suspicious areas all around the prostate.
- Look at a 3D image of the prostate during the procedure.
- Perform a complete prostate mapping.
- Keep a light and precise touch that diminishes the chance of infection and bleeding after the procedure.
Why have a prostate biopsy procedure?
Regardless of type, prostate biopsies are done whenever there’s reason to suspect prostate cancer. These reasons include:
- An elevated PSA (prostate-specific antigen) level, a kind of blood test that may indicate prostate cancer
- The presence of a suspicious lump during a digital rectal exam
- Unexplained blood in the urine or semen
- Abrupt difficulties urinating
By themselves, none of these symptoms can conclusively point to prostate cancer. Several are also classic symptoms of benign prostatic hyperplasia (BPH), more commonly known as an enlarged prostate, when the prostate slowly grows larger with age. However, the only way to know for sure is by examining the prostate tissue under a microscope.
Because traditional transrectal prostate biopsies often miss hidden tumors, it may be necessary to perform more than one biopsy before reaching a definitive cancer diagnosis. This is why patients with persistently high PSA levels but who’ve had a negative TRUS biopsy are often asked to repeat the procedure. In these cases, opting for a more accurate type of biopsy, such as a UroNav prostate biopsy, can make all the difference.
What to expect during a UroNav procedure?
Although the UroNav procedure requires relatively little time on the exam table, patients must take steps ahead of time to prepare, which can often be intimidating.
The first step is to undergo an MRI. This will be done a few days before the biopsy. MRIs are not painful, although they require you to fast for at least four hours before and lie still for an extended period. You may also need to receive a contrast dye before the MRI, which will be given intravenously.
During the days before the biopsy, your urologist may also ask you to:
- Stop taking blood-thinning medication, such as warfarin, aspirin, or ibuprofen (Advil).
- Provide a urine sample to rule out a urinary tract infection.
- Take a short course of antibiotics in some cases.
Finally, you must do a cleansing enema the evening before the biopsy.
You will receive a mild sedative and a local anesthetic on the day of the procedure. Then, you will lie on your side with your knees bent. You may experience discomfort while the doctor takes the biopsy samples, but the process will typically last less than 30 minutes.
What happens after the biopsy?
You can go home immediately after the biopsy, as long as someone else drives you, as the anesthetic can take a few hours to wear off completely.
You will need to avoid strenuous exercise for up to two days after the procedure, and you may feel some soreness. Some patients report seeing traces of blood in their stool or urine the day after a prostate biopsy. This is normal.
On the other hand, if you experience fever, heavy bleeding, or pain when urinating, you will be instructed to call the office immediately.
While the UroNav procedure has a lower risk of infection compared to a regular biopsy, it can still occur, so it’s best to be proactive and report any unusual side effects.
How long does it take to get the results from a biopsy, and what do they mean?
Waiting for the results from a prostate biopsy is often nerve-racking. Biopsy results typically take two or three days, but can occasionally take up to a week.
A negative result means the pathologist only found normal prostate cells. While reassuring, we may still need to monitor your PSA levels again or perform another digital exam in a few months.
The pathologist will find cancer cells in the tissue samples if the results are positive. However, the type of treatment that follows will depend upon your age and the “Gleason score.”
This test is a grading system for prostate cancer used to assess how aggressive the cancer is based on how abnormal the cells look under a microscope.
What does the Gleason score represent?
Tumors with a Gleason score under six are considered low-grade and may not need any immediate treatment, especially among older men. Instead, we may opt for active surveillance through regular blood tests and rectal exams, where we can monitor whether the cancer is growing.
Conversely, a Gleason score of 7 or higher indicates a high-grade cancer. If this occurs, we will refer you to an oncologist to discuss the most suitable treatment options.
Finally, the tissue sample analysis results may show another type of cell abnormality, such as prostatic intraepithelial neoplasia. These are not cancerous, but occasionally, they can become cancerous later on.
Depending on the type of abnormality and your risk factors, our urology team can monitor this with regular PSA tests, rectal exams, or even a follow-up biopsy.
Looking for prostate cancer screening in Los Angeles? Contact Tower Urology
Several of our urologists have been recognized by Newsweek as among the top prostate cancer surgeons in the nation, a testament to our team’s surgical expertise and patient-centered care.
Tower Urology’s board-certified urological team has been a leader in effectively treating cancer for over two decades, with specialists trained in all aspects of prostate health.
Tower Urology is a proud affiliate of Cedars-Sinai Medical Center, ranked #1 in California and #2 nationwide by U.S. News & World Report. This partnership reflects our dedication to delivering the highest standard of urologic care alongside the best urologists in Los Angeles.
Our years of experience and access to Cedars-Sinai’s world-class facilities ensure that our exceptional and innovative urological care positions Tower Urology as a leader in Southern California.
We invite you to establish a care plan with Tower Urology.
Tower Urology is conveniently located for patients throughout Southern California and the Los Angeles area, including Beverly Hills, Santa Monica, West Los Angeles, West Hollywood, Culver City, Hollywood, Venice, Marina del Rey, and Downtown Los Angeles.
Our services include treatment for bladder and urologic cancer, kidney cancer, prostate cancer, testicular cancer, and cancer fertility management.
Prostate Biopsy FAQs
The Gleason score and Grade group assess prostate cancer aggressiveness based on how abnormal cancer cells from tissue samples look under a microscope.
Gleason score
The Gleason score is derived from a biopsy’s two most common cell patterns (graded 1-5). These are added together (e.g., 3+4=7).
Scores indicate aggressiveness:
- <6: Low-grade
- 7: Intermediate (3+4 is less aggressive than 4+3)
- 8-10: High-grade
Grade group
The Grade group simplifies Gleason scores into five categories:
- 1: Gleason < 6
- 2: Gleason 3+4=7
- 3: Gleason 4+3=7
- 4: Gleason 8
- 5: Gleason 9-10
These systems guide treatment and predict cancer progression.
The prostate is a small, walnut-shaped gland found only in males, located below the bladder and in front of the rectum. It’s part of the male reproductive system and produces fluid that forms part of semen. Prostate cancer is a disease in which cells in the prostate gland grow uncontrollably.
Sources
What is Prostate Cancer?
https://www.cancer.org/cancer/types/prostate-cancer/about/what-is-prostate-cancer.html
Prostate Cancer Basics
https://www.cdc.gov/prostate-cancer/about/index.html