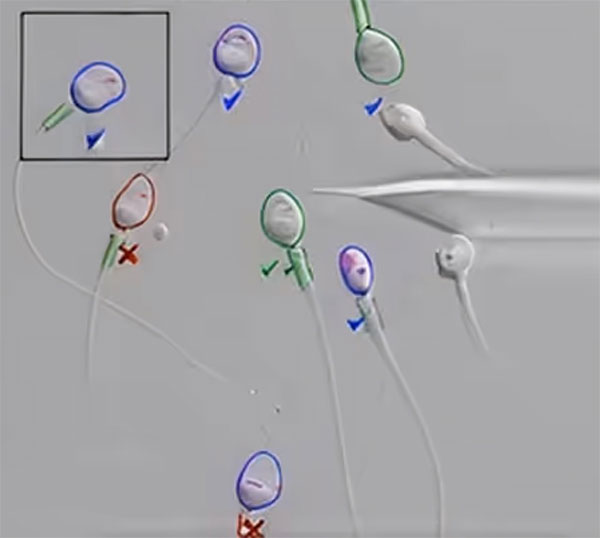
We’re revolutionizing men’s fertility testing with AI Technology, one cell at a time.
Tower Urology’s in-house male fertility testing lab offers our patients an innovative solution that seamlessly integrates advanced hardware and intelligent software to deliver fast, accurate, and reliable results.
With 95% accuracy in cell analysis, our system achieves high accuracy in sperm count prediction, significantly surpassing traditional manual methods.
As a result of our new lab, Tower Urology patients receive results in minutes, rather than days, because we don’t need to send samples to an off-premises third-party lab.

What is a semen analysis test?
It is estimated that male factor infertility affects up to 15% of men of reproductive age in the US and that male factors contribute to approximately half of all infertility cases. Yet, it seems that fertility clinics and conversations around reproductive medicine generally focus much less on fertility treatments for men.
Hormone imbalances, DNA fragmentation (where the sperm nucleus is damaged), injury, or infection are just a few of the many and varied reasons for male infertility issues. However, the first and most important step in any man’s fertility evaluation.
Semen is the fluid that a man ejaculates. It consists of sperm, prostatic secretions, and seminal vesicle secretions — approximately 75% from seminal vesicles, 23% from the prostate, and about 2% of sperm from the testicles.
While the sperm are the cells responsible for fertilizing an egg, the health of the surrounding fluid is equally important for sperm function. Therefore, we evaluate both the sperm and the fluid in our analysis.
It is important to remember that there are no perfect results, just like there is no magic number of sperm concentration (sperm count) that will guarantee pregnancy. Some men with poor semen analyses may still conceive, while others with excellent results may not. However, men with healthy semen parameters generally have significantly higher conception rates.
Ultimately, a semen analysis can help determine if a male factor is contributing to a couple’s fertility challenges and help your fertility doctor decide whether a more detailed evaluation is needed.
What does a standard semen analysis include?
Most laboratories report on the following parameters according to World Health Organization guidelines:
- Concentration: Number of sperm per milliliter. Normal: >60 million/cc. Sub-fertile: <20 million cc.< li>
- Motility: Percentage of sperm that are moving. Normal: ≥50%.
- Morphology: Percentage of normally shaped sperm. Normal: ≥30%.
- Volume: Normal ejaculate volume is ≥2 mL.
- Total motile count: Number of moving sperm in the entire sample. Ideal: >40 million motile sperm.
Fluid characteristics: Color, viscosity, and liquefaction time are all factors considered in the analysis, as these are all critical for sperm function.
Tower Urology’s advanced fertility analysis
At Tower Urology, we go far beyond the standard semen test. We utilize next-generation fertility analysis tools that combine the latest AI-driven technologies with biomarker testing to reveal a more comprehensive picture of a man’s fertility potential.
These cutting-edge advancements enable us to:
- Accurately quantify and monitor subtle abnormalities in sperm morphology (shape), motility (movement), and concentration (count).
- Detect previously unmeasurable molecular indicators of fertility.
- Personalize infertility treatment strategies based on a patient’s unique sperm profile.
Our advanced semen diagnostics might include:
- Forward progression: Tracks how effectively sperm are moving forward, not just whether they’re moving.
- Kruger morphology: Uses high-magnification imaging to assess the detailed structural integrity of sperm.
- Antisperm antibodies: Detects immune reactions that can impair sperm function and egg penetration.
- White blood cell detection: Identifies inflammation or infection, which is often overlooked in routine laboratory tests.
- Spun specimen testing: Helps uncover extremely low sperm counts that might be missed on initial review.
- Sperm viability: Determines what percentage of non-motile sperm are still alive.
- Fructose testing: Helps distinguish between production issues and ejaculatory blockages.
- Post-ejaculatory urinalysis(PEU): Identifies retrograde ejaculation by analyzing urine after orgasm.
These test results provide deeper insights, enabling our fertility specialists to recommend suitable treatment options and create personalized treatment plans for each patient.
Why choose Tower Urology in Los Angeles for a semen analysis test near you?
At Tower Urology, we help men take control of their reproductive health. Our advanced fertility testing provides the most comprehensive understanding of your current fertility and potential fertility, utilizing the latest technology in AI and biomarker-based testing.
We combine precise diagnostics with world-class expertise in male fertility to provide our patients with every advantage, whether they are trying to conceive naturally or preparing for advanced reproductive technologies.
Our physicians are fellowship-trained specialists in male fertility and reproductive medicine. Our state-of-the-art laboratory is equipped with AI-enabled analysis tools, delivering faster, deeper, and more accurate results, as well as more actionable insights than traditional methods.
The advantage of Tower Urology lies in our unwavering commitment to providing world-class urologic care through advanced technology, personalized treatment plans, and a patient-centered approach. With a reputation for excellence and innovation, we deliver superior outcomes that distinguish us as leaders in urologic health.
Tower Urology is a proud affiliate of Cedars-Sinai Medical Center, ranked #1 in California and #2 nationwide by U.S. News & World Report. This partnership reflects our dedication to delivering the highest standard of urologic care alongside the best urologists in Los Angeles. Our years of experience and access to Cedars-Sinai’s world-class facilities ensure that our exceptional and innovative urological care positions Tower Urology as a leader in Southern California.
We invite you to establish a care plan with Tower Urology. Please make an appointment online or call us at (310) 854-9898.
Tower Urology is conveniently located for patients throughout Southern California and the Los Angeles area, including Beverly Hills, Santa Monica, West Los Angeles, West Hollywood, Culver City, Hollywood, Venice, Marina del Rey, and Downtown Los Angeles.