What is a no-scalpel vasectomy?
A no-scalpel vasectomy procedure is a modern, minimally invasive, outpatient surgical procedure. The goal is to provide a permanent form of birth control for men who no longer wish to father children. It is a highly effective, long-term solution for preventing pregnancy without the need for ongoing contraceptives.
This procedure does not require general anesthesia. It has minimal recovery time, side effects, and discomfort during and after the procedure.
At Tower Urology, we specialize in this advanced technique, offering men a safe, effective, and virtually painless option for family planning.

Who is the ideal candidate for a no-pain, no-needles, no-scalpel vasectomy?
The ideal candidate for a no-pain, no-needles, no-scalpel vasectomy is a man who:
- Is certain he does not want children in the future.
- Seeks a minimally invasive, quick, and effective procedure for permanent contraception.
- Prefers a method with little to no discomfort, quick recovery, and no impact on sexual function.
- Desires a reliable alternative to temporary contraception methods, such as condoms or hormonal birth control, for their partner.
How is the Tower Urology no-scalpel vasectomy performed?
Our no-scalpel vasectomy involves the following steps:
No needle anesthesia
A local anesthetic is administered using a jet injector, eliminating the need for traditional needles.
No scalpel technique
A small opening is made in the scrotum using specialized instruments instead of a traditional incision.
Sealing the vas deferens
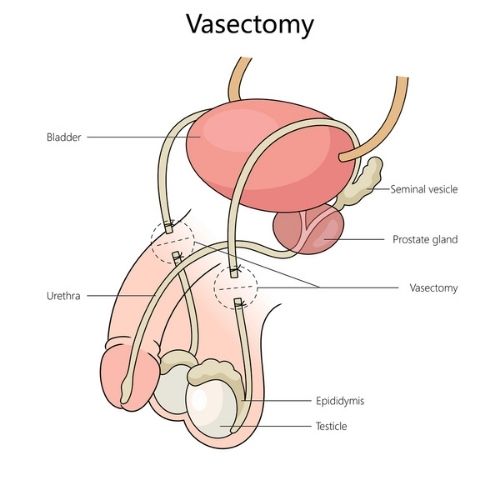
Your doctor will gently stretch the skin of this opening to see your vas deferens (the tubes that carry sperm). These tubes are then sealed and returned to their position.
Quick and minimally invasive
The entire procedure takes less than 30 minutes. Since the opening is small, stitches are not needed.
How effective is the no-scalpel vasectomy?
A no-needle, no-scalpel vasectomy is highly effective, with success rates exceeding 99%, comparable to traditional vasectomy methods. It is the most reliable method available for preventing pregnancy. This less invasive technique results in less pain, bleeding, and infection, as well as faster recovery and lower complication rates, typically less than 1%.
The method of anesthesia and the absence of incisions do not affect its effectiveness; the key factor is the occlusion (sealing) of the vas deferens, which is consistent across techniques. However, sterility is not immediate, so alternative contraception is needed until a semen analysis confirms the absence of sperm.
How safe is the no-scalpel vasectomy?
This procedure is highly safe, but as with any medical intervention, there are minimal risks, including:
- Mild discomfort at the surgical site.
- A rare instance of failure.
At Tower Urology, our advanced techniques and expertise minimize these risks, ensuring a smooth experience for our patients.
What is the recovery from a no-scalpel vasectomy like?
It’s a quick recovery
Most men can return to work and engage in light physical activity within one to two days.
You’ll have minimal discomfort
You may feel some mild pain, temporary swelling or bruising, and, in rare instances, bleeding or infection at the surgical site. We recommend applying an ice pack intermittently to your underwear or athletic supporter covering your scrotum for the first 24 hours. Over-the-counter medications and ice packs can typically manage any mild discomfort.
Sexual activity can usually be resumed after one week
However, it’s essential to use contraception until a follow-up semen analysis confirms the absence of sperm with ejaculation.
Are there other procedures to consider that offer the same benefit?
There are two types of vasectomy surgeries available today. The first is our no-scalpel vasectomy, which requires just a small puncture. This is the most advanced and minimally invasive option for permanent male contraception. The other option is a traditional vasectomy, which involves small incisions and sutures around the testicles and achieves the same result.
What is the difference between a no-scalpel vasectomy and a traditional vasectomy?
Both types of male sterilization procedures, non-scalpel and conventional vasectomy scalpel procedures, achieve the same goal—permanent male birth control by cutting or sealing the tubes (vas deferens) that carry sperm. The difference is in how the procedure is performed.
In a scalpel vasectomy, the doctor makes one or two minor cuts in the skin of the scrotum using a surgical scalpel to access the tubes. In a no-scalpel vasectomy, the doctor uses a special tool to make a tiny puncture in the skin instead of cutting it. This means less bleeding, a lower risk of infection, and typically less pain, as well as a quicker recovery.
What type of vasectomy is the best?
Both a conventional scalpel vasectomy and a no-scalpel vasectomy can be performed under local anesthesia in the urologist’s office or at an outpatient surgery center, and the patient can go home the same day.
Both methods are highly effective, with a near-zero failure rate. However, the no-scalpel approach is often preferred because it is minimally invasive, carries a lower risk of infection and hematoma, involves fewer complications, and allows patients to return to normal activities more quickly. Multiple studies have also shown that the no-scalpel method offers better vas occlusion, i.e., sealing of the vas deferens. This results in a lower failure rate than other sealing forms, such as simple suture or clip ligation.
Important advice for patients considering a vasectomy
If you’re considering a no-scalpel vasectomy, we remind patients that this is a permanent decision. While a traditional vasectomy can be reversed with the vasectomy reversal procedure, the success rate is by no means guaranteed. As a result, we recommend that you consider a vasectomy to be permanent.
Please take the time to discuss your goals and family planning needs with your partner and our team.
Many men find it empowering to take control of their reproductive health, and this procedure offers a convenient, reliable solution with minimal impact on their daily lives.
Why choose Tower Urology in Los Angeles for your no-scalpel vasectomy?
At Tower Urology, we take a personalized, evidence-based approach to general urology care. All our professionals are committed to providing expert care and follow-up. We take the time to understand you and personalize your treatment plan to your needs.
We invite you to establish care with Tower Urology.
Tower Urology is a proud affiliate of Cedars-Sinai Medical Center, ranked #1 in California and #2 nationwide by U.S. News & World Report. This partnership reflects our dedication to delivering the highest standard of urologic care alongside the best urologists in Los Angeles. Our years of experience and access to Cedars-Sinai’s world-class facilities ensure that our exceptional and innovative urological care positions Tower Urology as a leader in Southern California.
Tower Urology is conveniently located for patients throughout Southern California and Los Angeles, including Beverly Hills, Santa Monica, West Los Angeles, West Hollywood, Culver City, Hollywood, Venice, Marina del Rey, Burbank, Glendale, and Downtown Los Angeles.
Our services include treatment for low testosterone, chronic pelvic pain, chronic testicular pain, and Peyronie’s disease.
No-scalpel vasectomy FAQs
A vasectomy is generally considered a safe procedure with a low risk of long-term problems. Most men do not experience noticeable side effects, and serious health issues are rare.
However, some potential long-term complications include chronic testicular pain, known as post-vasectomy pain syndrome (PVPS). This affects about 1-2% of men and can last months or years.
There is also concern about possible associations with prostate cancer, but current evidence does not establish a definitive link. Additionally, rare issues such as delayed vasectomy failure, sperm granulomas, or vasovenous fistulas may occur.
Overall, long-term physiological health, including hormone levels and cancer risk, appears unaffected, but psychological effects and chronic pain are potential concerns.
Current research shows that vasectomy is linked to a slight increase in the risk of being diagnosed with prostate cancer (about 10–18% higher relative risk). However, the absolute risk increase is very low, and studies do not show a higher risk of aggressive or fatal prostate cancer after vasectomy. Most medical organizations do not consider this a reason to avoid vasectomy, but it’s a good idea to discuss any concerns with your doctor.
A vasectomy does not affect your sex drive or ability to get erections. Your testosterone levels and sexual function remain the same because only the tubes that carry sperm are cut—nothing else changes. Most men notice no difference in libido or erections after the procedure. If you do experience changes, it’s usually due to stress or unrelated issues, not the vasectomy itself.
The cost of a no-scalpel vasectomy in the United States typically ranges from $500 to $1,300 if you are paying out of pocket. Depending on your location and provider, some clinics may charge as low as $300 or as high as $1,500. Most health insurance plans cover part or all of the cost, so your out-of-pocket expense could be limited to a copay or coinsurance if you have coverage. Medicaid and some state programs may also cover the procedure for eligible individuals, potentially making it free or very low cost.
Sources
Vasectomy: AUA Guideline
https://doi.org/10.1016%2Fj.juro.2012.09.080
A Review of 10 Years of Vasectomy Programming and Research in Low-Resource Settings | Global Health: Science and Practice
https://doi.org/10.9745%2FGHSP-D-16-00235
Vasectomy Regret or Lack Thereof
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9476225
Scalpel versus no‐scalpel incision for vasectomy
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6464377
































































