What is benign prostatic hyperplasia?
Benign prostatic hyperplasia (BPH) is a noncancerous enlargement of the prostate gland. It is the most common benign tumor found in men. As with prostate cancer, BPH is more prevalent in Western countries, such as the United States, than in Eastern countries, such as Japan and China.
What are the common symptoms of an enlarged prostate (BPH)?
- Weak or interrupted urine flow
- Difficulty starting urination (hesitancy)
- Dribbling at the end of urination
- Straining to urinate
- Incomplete bladder emptying
- High urinary frequency
- Nocturia (the need to urinate during the night)
- Urgency
- Acute urinary retention
- Pain or discomfort during urination
- Urinary Incontinence
How do we diagnose BPH?
When you attend as a new patient for the first time, we take a detailed medical history, review your existing medical records, and conduct a physical examination.
After that, several methods can be used to diagnose BPH. These include:
- A prostate-specific antigen (PSA) blood test.
- A post-void residual test (ultrasound measurement of how much urine is left behind) and flow studies.
- A cystoscopy exam is necessary to investigate red-flag symptoms, such as unexplained hematuria (the presence of blood in the urine), possible bladder calculi (stones in the bladder), and suspected bladder cancer, to determine the degree of obstruction in the prostatic urethra and evaluate the bladder for stones and signs of damage.
Cystoscopy provides a reasonable estimate of prostate size and shape, can assess the degree of obstruction, and visually represents any signs of bladder damage. - An American Urological Association (AUA) symptom score. We also utilize an outcome tracker called “OutcomeMD.” This utilizes continuously updated questionnaires to monitor and evaluate changes in our patients’ symptoms and treatment outcomes.
What are the treatment options for BPH?
If you have been diagnosed with benign prostatic hyperplasia, there are several treatment options to consider. We will work with you to determine the best course of action and devise a treatment plan that will take into account the severity of your symptoms, the size of your prostate, and your overall health.
If your symptoms are mild, we may recommend watchful waiting. This means scheduling regular examinations to evaluate your symptoms on an ongoing basis rather than treating the condition.
However, we will likely recommend treatment if your symptoms are moderate to severe. BPH treatment options fall into three categories:
- Medications
- In-office procedures
- Surgical procedures
What medications are typically prescribed for BPH?
Several medications are available to treat benign prostatic hyperplasia (BPH). These medications work by relaxing the muscles in the prostate and bladder, which can help relieve mild symptoms such as frequent urination and difficulty urinating.
Common medications include:
Alpha-blockers
These medications relax the muscles in the prostate and the bladder neck, making urination easier. Examples include tamsulosin (Flomax), alfuzosin (Uroxatral), Rapaflo (silodosin), and Hytrin (terazosin).
Side effects of alpha-blockers may include dizziness, lightheadedness, and retrograde ejaculation (in which semen enters the bladder instead of exiting the penis during ejaculation).
5-alpha reductase inhibitors
These medications shrink the prostate by blocking the production of a hormone called dihydrotestosterone (DHT). Examples include finasteride (Proscar) and dutasteride (Avodart).
Side effects of 5-alpha reductase inhibitors may include decreased sex drive, erectile dysfunction, and breast enlargement or tenderness.
Combination medications
Some medications combine an alpha-blocker with a 5-alpha-reductase inhibitor. Examples include Jalyn (dutasteride and tamsulosin) and Combodart (dutasteride and alfuzosin).
Combination medications may have side effects from both alpha-blockers and 5-alpha reductase inhibitors.
Daily Cialis (tadalafil)
Tadalafil is also sometimes prescribed as a treatment for BPH. It works by relaxing the muscles in the bladder and prostate, which can help improve urine flow. Cialis is a type of phosphodiesterase type 5 inhibitor (PDE5 inhibitor), which also helps increase blood flow to the penis and is used to treat erectile dysfunction.
Side effects of Daily Cialis (tadalafil) may include headache, indigestion, and back pain.
Other medications that may contribute to helping BPH symptoms
In addition to the drugs referred to above that treat BPH directly, other medications can be used as combination therapy to help improve the conditions associated with BPH.
The following medications all treat the symptoms of an overactive bladder (OAB), such as frequent urination, sudden urges to urinate, and leakage. They work by relaxing the bladder muscles, which helps to reduce these symptoms and improve bladder control. These medications include:
- Oxybutynin (Ditropan XL)
- Mirabegron (Myrbetriq)
- Tolterodine (Detrol)
- Solifenacin (Vesicare)
- Vibegron (Gemtesa)
In older adults, the side effects of Ditropan, Detrol, and Vesicare may include dry mouth, constipation, blurred vision, and confusion.
Side effects unique to Myrbetriq include an increase in blood pressure.
Additionally, some medications may cause urinary retention or difficulty urinating, which can worsen BPH symptoms.
What minimally invasive procedures are available to treat benign prostatic hyperplasia?
If medications do not provide adequate relief, or you are averse to taking drugs, we may recommend an office-based procedure. All these procedures can be performed in our office. Although general anesthesia is not required, we recommend administering Valium IV and using nitrous oxide to help alleviate any pain or discomfort during the procedure.
While office-based procedures generally have fewer risks than more invasive surgeries, any intervention procedure relating to the prostate can cause erectile dysfunction, incontinence, retrograde ejaculation, and irritative symptoms. When considering treatment options for BPH, discussing these issues, the potential risks, and what is essential for you and your quality of life is important.
Examples of office-based procedures include:
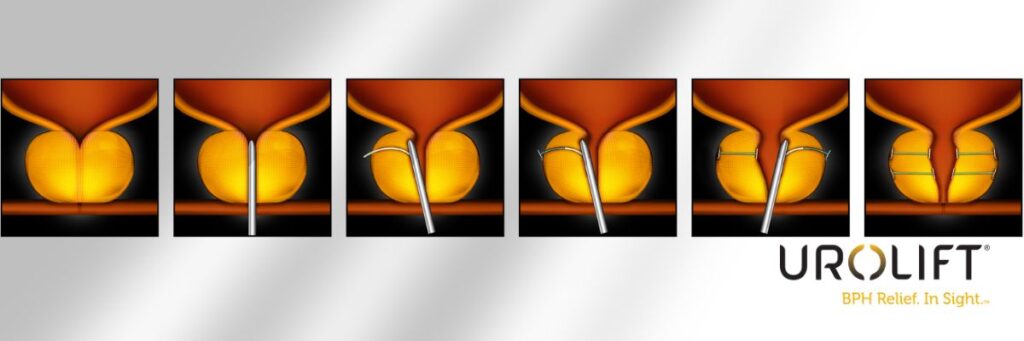
UroLift
This procedure involves inserting small metallic implants into the prostate to lift and hold the enlarged tissue out of the way. This opens the urethra and improves urine flow. Learn more about UroLift.
What are the advantages of UroLift?
- The procedure is minimally invasive.
- It can be performed in our office.
- General anesthesia is not required.
- It typically provides rapid symptom relief.
- It does not cause retrograde ejaculation and can prevent infertility.
What are the disadvantages of UroLift?
- There can be some pain or discomfort during the procedure.
- It may cause urinary tract infections (UTIs) or difficulty urinating shortly after the procedure.
- It may not be enough to relieve the obstruction if you have a very long or large prostate, and you may subsequently require a more invasive procedure to remove the implants and the obstructed gland.
Who should not try UroLift?
If you have a very large prostate (above 80 grams), have a prominent median lobe, or have bladder stones or bladder tumors, UroLift is not recommended.
What should I expect after a UroLift procedure?
Most patients experience rapid symptom relief and can return to normal activities within a few days. However, some patients may experience mild pain or discomfort during urination for a few days afterward, especially if we leave a catheter post-procedure.
The Rezum Procedure
The Rezum procedure uses hot steam to shrink the prostate tissue, relieving pressure on the urethra and improving urine flow.
What are the advantages of Rezum water vapor therapy?
- The procedure is minimally invasive.
- It can be performed in our office.
- General anesthesia is not required.
- It typically provides rapid symptom relief.
- It can treat a median lobe if present.

What are the disadvantages of Rezum?
- You may experience pain or discomfort during the procedure.
- It can cause retrograde ejaculation.
- It may cause UTIs or difficulty urinating shortly after the procedure.
Who is not a good candidate for the Rezum procedure?
Rezum is not recommended for patients with very large prostates, above 80 grams, or those with bladder stones. It is also contraindicated in patients who have had an artificial urinary sphincter or those with an inflatable penile prosthesis. Patients with a history of radiation treatment involving the prostate are not ideal candidates for Rezum.
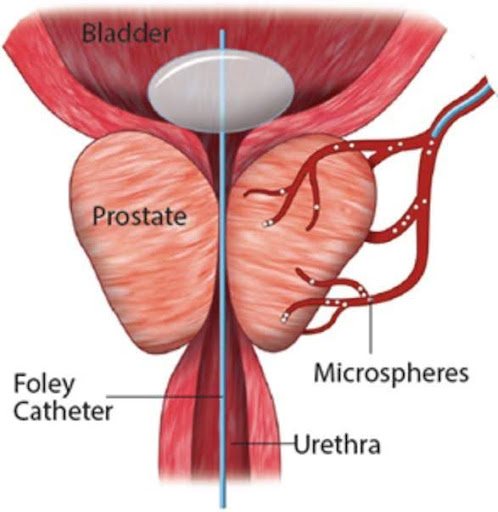
Prostate artery embolization
Prostate artery embolization (PAE) is an outpatient procedure that blocks the blood supply to the prostate, causing it to shrink and improving urine flow. An interventional radiologist typically performs procedures such as an angiogram of the heart.
Unlike the transurethral resection of the prostate (TURP) procedure (see below), which requires general anesthesia, PAE is performed under light sedation.
This therapy takes some time to take effect, so if you require rapid improvement in your symptoms, this may not be the ideal option for you. But don’t be concerned, as your Tower Urology physician will review each option’s benefits and drawbacks as you chart the best course of action together.
The effects of treatment may last 15 years or longer. Follow-up treatment may be necessary to alleviate symptoms, especially after several years have passed.
iTIND (Temporarily Implanted Nitinol Device)
The iTIND is a minimally invasive option that involves inserting a small probe into the prostate and using radiofrequency energy to heat and destroy excess tissue. The advantages of the iTIND include the ability to perform the procedure in-office under local anesthesia, without the need for a hospital stay or general anesthesia.
This procedure is typically well-tolerated and can provide significant relief from BPH symptoms. However, like other procedures, there are some risks associated with iTIND, including the possibility of urinary retention, difficulty urinating, and retrograde ejaculation. Additionally, some patients may experience mild pain or discomfort during and after the procedure.
iTIND is a relatively new procedure, and long-term success data are somewhat limited.
Microwave therapy
Microwave therapy is a minimally invasive procedure that uses microwaves to destroy excess prostate tissue and relieve pressure on the urethra. During the procedure, a small probe is inserted into the prostate, and microwaves are used to heat and destroy the tissue.
This procedure is typically well-tolerated and can provide significant relief.
However, like other procedures, microwave therapy has some risks, including the possibility of urinary retention, difficulty urinating, and retrograde ejaculation. Additionally, long-term data on its effectiveness are limited compared to other procedures.
Due to its limited long-term success, microwave therapy has largely been abandoned. Nowadays, most patients who are considering an in-office-based ablation procedure undergo Rezum.
What surgical treatments are available for BPH?
In severe cases, prostate surgery may be necessary to treat BPH, including minimally invasive endoscopic procedures and more invasive surgeries to treat different-sized prostates.
All the following procedures require anesthesia in a hospital or surgery center. Sometimes, you can go home on the same day of the procedure. These procedures include:
Transurethral resection of the prostate
Transurethral resection of the prostate (TURP) involves removing the inner portion of the prostate using a resectoscope inserted through the urethra. This operation is typically reserved for prostates in the size range between 30 mL and 80 mL. The advantages of this operation are that it can be done under spinal anesthesia (epidural), there are no incisions, and the catheter typically remains in place for only 2-3 days, though sometimes just overnight. This procedure does not affect sexual function.
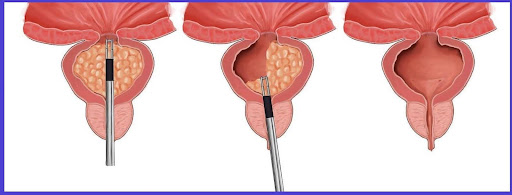
What are the disadvantages of the TURP procedure?
Disadvantages include the limited size of the prostate that we can resect. Like other interventions for BPH, the side effects may include urinary incontinence, irritative symptoms, and erectile dysfunction. Given advances in technology over the past decade, however, these risks are very low and can be mitigated due to the type of technology used for the resection.
Most TURP procedures are performed using bipolar energy, which has significantly lower rates of complications compared to TURP procedures using traditional monopolar cautery.

Holmium laser enucleation of the prostate
Holmium laser enucleation of the prostate (HoLEP) is a urological surgery that uses a laser to remove the excess prostate tissue and relieve pressure on the urethra.
Robotic aquablation
Robotic aquablation is a minimally invasive surgical option for treating BPH. This procedure involves using a robot to deliver a high-pressure water jet to remove excess prostate tissue. The robot utilizes real-time ultrasound imaging to guide the water vapor jet, ensuring precise tissue removal while minimizing damage to surrounding structures.
Robotic aquablation is typically reserved for patients with larger prostates who may not be ideal candidates for other minimally invasive procedures.
What are the advantages of robotic aquablation?
The advantages of this procedure include reduced risk of complications such as sexual dysfunction and incontinence, maintenance of anterograde ejaculation, and reduced recovery time compared to traditional open surgeries. There is also reduced blood loss, no incisions, and faster recovery.
Although advances in robotic surgery have improved visualization of the operative field, as with any surgical procedure, robotic ablation has some risks, including the possibility of bleeding, infection, and urinary retention.
Open simple prostatectomy
Open simple prostatectomy (OSP) surgery involves an open incision in the lower abdomen to remove the inner portion of the prostate. This procedure is typically reserved for patients with very large prostates or those with a significant median lobe.
What are the disadvantages of open simple prostatectomy?
Open surgery can lead to a longer hospital stay, greater blood loss, and an increased risk of complications. For this reason, most top-level surgeons have abandoned open surgery procedures and now favor the use of state-of-the-art robotic technology to manage very large glands.
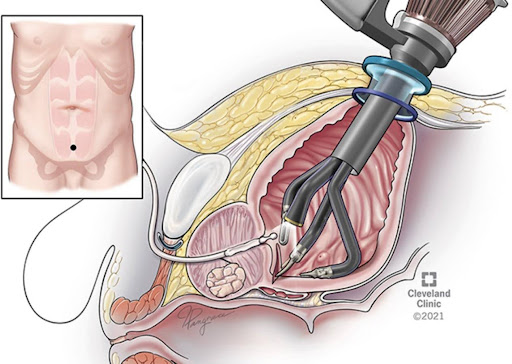
Robotic simple prostatectomy
Robotic simple prostatectomy surgery involves removing the inner portion of the prostate using a robotic device, which allows for far greater precision and control compared to open surgery.
It is also associated with a reduced risk of complications such as sexual dysfunction and incontinence. It is typically reserved for very large prostates or those with a significant median lobe.
What are the advantages of robotic simple prostatectomy?
Robotic simple prostatectomy is a minimally invasive option for patients with very large prostates with a greatly reduced risk of complications like incontinence and sexual dysfunction.
More recently, the most significant advancement in robotic technology has been the single-port device, which enables all instruments to be placed within the bladder cavity through an incision of less than 3 cm, allowing for the procedure to be carried out.
A single entrance incision minimizes post-operative pain and also allows us to easily extract the resected adenoma (prostate tissue), minimizing time under anesthesia.
Depending on your prostate size and anatomy, we will determine which approach is more suitable for your case.
Why trust Tower Urology for your benign prostatic hyperplasia care?
Tower Urology’s board-certified urological team has been a leader in successfully treating BPH for over two decades, with specialists trained in all aspects of prostate health. All our professionals at Tower Urology are dedicated to providing you with expert care. We take the time to understand you and personalize your treatment plan to your needs.
Tower Urology’s advantage lies in our unwavering commitment to providing world-class urologic care through advanced technology, personalized treatment plans, and a patient-centered approach. With a reputation for excellence and innovation, we deliver superior outcomes that set us apart as a leader in urologic health.
Tower Urology is a proud affiliate of Cedars-Sinai Medical Center, ranked #1 in California and #2 in the nation by U.S. News & World Report. This partnership reflects our commitment to delivering the highest standard of urologic care with the best urologists in Los Angeles. Our years of experience and access to Cedars-Sinai’s world-class facilities and our exceptional, innovative, and state-of-the-art urological care make Tower Urology a leader in Southern California.
Tower Urology is conveniently located for patients throughout Southern California, including the Los Angeles area, as well as Beverly Hills, Santa Monica, West Los Angeles, West Hollywood, Culver City, Hollywood, Venice, Marina del Rey, and Downtown Los Angeles.
Other related conditions and treatments we provide include therapy for enlarged prostate (BPH), Rezum procedure, robotic prostatectomy, and UroLift, to name a few.
FAQs About Benign Prostatic Hyperplasia (BPH)
Benign prostatic hyperplasia (BPH) is common, especially as men age. About half of men in their 50s start experiencing some symptoms, and this increases to up to 90% of men over the age of 80. It’s a normal part of getting older, and many men go through it at some point in their lives. If you’re experiencing any symptoms, it’s a good idea to talk to your urologist or healthcare provider, as effective treatments are available.
Absolutely! By effectively managing your symptoms with our healthcare professionals, you can live a normal life with BPH. Many men with BPH lead active, healthy lives by working closely with their healthcare providers to find the proper treatment, which may include medications, lifestyle changes, or minimally invasive procedures. Simple adjustments like reducing evening fluid intake, limiting caffeine and alcohol, and practicing regular bathroom schedules can help alleviate discomfort.
Additionally, staying physically active and maintaining a healthy, balanced diet can support overall urinary health. With proper care and attention, BPH symptoms can be controlled, allowing you to continue your daily activities without significant disruptions./
There’s no strong scientific evidence that ejaculation alleviates the symptoms of an enlarged prostate (benign prostatic hyperplasia or BPH). While maintaining a healthy sexual routine can be part of overall well-being, it’s important to consult with our urologist for truly effective treatments and management strategies for an enlarged prostate.
The leading cause of BPH is the natural aging process in men. As men get older, hormonal changes occur, particularly involving the levels of testosterone and its byproduct, dihydrotestosterone (DHT). These hormonal shifts cause the prostate gland to gradually enlarge, which can press against the urethra and lead to common urinary symptoms such as difficulty starting to urinate or needing to go more frequently.h
BPH itself typically does not affect a man’s life expectancy, as it’s a noncancerous enlargement of the prostate that mainly causes urinary symptoms. Most men with BPH live normal, healthy lives with proper management and treatment, such as medications or procedures to relieve symptoms.
There are some natural remedies that our patients find helpful in managing the symptoms of an enlarged prostate (BPH). Supplements like saw palmetto, beta-sitosterol, and pygeum are commonly used and may help reduce urinary issues by improving urine flow and decreasing inflammation.
However, the effectiveness of these natural treatments can vary from person to person, and it’s important to consult with a urologist before starting any new remedy to ensure it’s safe and suitable for your specific needs.
Additionally, lifestyle changes can be made that can be of significant benefit. These include curbing caffeine, alcohol, and tobacco, increasing exercise, and eating better. For some patients, dealing with their obesity can also pay great dividends.ad
Sources
Enlarged Prostate (Benign Prostatic Hyperplasia)
https://www.niddk.nih.gov/health-information/urologic-diseases/prostate-problems/prostate-enlargement-benign-prostatic-hyperplasia
Incidence and prevalence of lower urinary tract symptoms suggestive of benign prostatic hyperplasia in primary care–the Triumph project
https://pubmed.ncbi.nlm.nih.gov/12361895
Serenoa repens for the treatment of lower urinary tract symptoms due to benign prostatic enlargement
https://pubmed.ncbi.nlm.nih.gov/37345871
Phytotherapy for lower urinary tract symptoms secondary to benign prostatic hyperplasia
https://pubmed.ncbi.nlm.nih.gov/18423748
Beta‐sitosterols for benign prostatic hyperplasia
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8407049
































































