What is prostatitis?
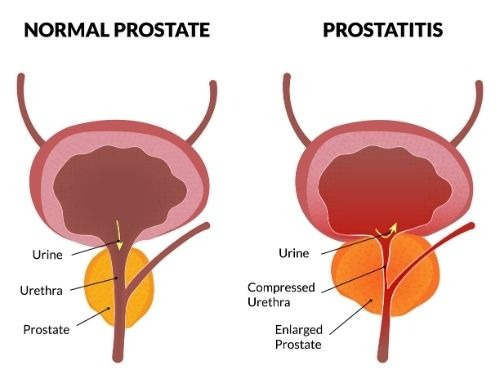
The prostate is a small, walnut-shaped gland located just below the bladder and in front of the rectum in men. The National Institute of Health has a good image of where the prostate is located. Inflammation or infection of the prostate is called prostatitis.

What are the symptoms of prostatitis?
Inflammation of the prostate gland can cause a variety of uncomfortable symptoms. These include:
- Pain in your genital area (often in the area between your scrotum and anus), your lower abdomen, and/or your lower back.
- There might also be pain in your penis and testicles.
- Painful or difficult urination.
- Erectile dysfunction, such as painful ejaculation.
- Flu-like symptoms such as a fever and chills.
What types of prostatitis are there, and what causes them?
There are four types of prostatitis. The causes vary depending on the type.
- Acute bacterial prostatitis: This acute prostatitis is caused by a sudden bacterial infection. Examples are bacteria (for example, E. coli) from a urinary tract infection (UTI) or sexually transmitted infections (STIs) like chlamydia or gonorrhea.
- Chronic bacterial prostatitis: Results from a persistent (recurring) bacterial infection, often following an untreated acute episode.
- Chronic prostatitis / Chronic pelvic pain syndrome (CPPS): CPPS is the most common type. Unfortunately, the causes are unclear, possibly linked to stress, nerve damage, or immune responses.
- Asymptomatic inflammatory prostatitis: Often discovered incidentally, this type of inflammation has no symptoms or apparent trigger.
Who does prostatitis normally affect?
Prostatitis can affect men of all ages, but it’s most common in men aged 30–50. It’s the leading urologic issue for men under 50. It is also highly common in older age groups, often overlapping with conditions like benign prostatic hyperplasia (BPH). BPH is a noncancerous enlargement of your prostate gland.
At Tower Urology, we see a wide range of patients, from young adults with acute bacterial prostatitis to older men managing chronic pelvic pain syndrome (CPPS). Our professional and caring team is equipped to help regardless of your age or symptoms.
What are the common risk factors of prostatitis?
Risk factors include:
- Recent UTI or bladder infection.
- Use of a urinary catheter.
- Pelvic trauma or injury.
- High-risk sexual practices (for example, unprotected anal sex).
- Enlarged prostate (BPH) in men over 50.
- History of prostatitis.
How do you generally diagnose prostatitis?
Diagnosing prostatitis requires a thorough approach. At Tower Urology, we use advanced tools to ensure accuracy:
- Medical history & physical exam: Your expert healthcare provider will take a complete medical history. Then, we will assess your symptoms and perform a digital rectal exam (DRE) to check for prostate tenderness or swelling.
- Urine tests: We use urinalysis and urine cultures to identify bacterial infections.
- Prostate fluid analysis: While doing a digital rectal exam (DRE), we will pay attention to any fluid that comes out. This fluid can reveal signs of inflammation or the presence of bacteria.
- Imaging: Ultrasound or MRI may rule out abscesses or other issues.
- Urodynamic tests: These will be used to evaluate your bladder and urethral function if urinary symptoms persist.
What are the treatment options for prostatitis?
Treatment approaches vary depending on the type of condition. Treatments may include antibiotics for bacterial infections, alpha blockers to relax muscles, anti-inflammatory medications, and lifestyle changes such as avoiding certain foods and beverages that may irritate the prostate.
More specifically, here are treatments for prostatitis types:
- Acute bacterial prostatitis: Antibiotics (e.g., fluoroquinolones) for 2–6 weeks, sometimes with IV therapy for severe cases. Pain relief and hydration support recovery.
- Chronic bacterial prostatitis: Longer antibiotic courses (4–12 weeks) to eradicate (wipe out) deep-seated infections.
- Chronic Pelvic Pain Syndrome (CPPS): A multimodal approach including anti-inflammatory drugs, alpha-blockers, physical therapy, and stress management. Antibiotics may be trialed initially.
- Asymptomatic inflammatory prostatitis: Typically requires no treatment unless related to other conditions.
Are there treatments Tower Urology offers that other practices generally don’t?
Yes! At Tower Urology, we go beyond standard care:
- Pelvic floor physical therapy: For CPPS, we offer specialized treatment for your pelvic floor muscles. This therapy works to reduce muscle tension and nerve irritation. Other practices often overlook this treatment.
- Advanced Pain Management: Our urologists collaborate with pain specialists to provide cutting-edge options, such as nerve blocks or biofeedback.
- Holistic stress management: We integrate counseling and relaxation techniques, recognizing the link between stress and CPPS symptoms.
Are there treatments at other practices that Tower Urology generally doesn’t do?
We avoid outdated or unproven methods such as:
- Routine prostate massage: While some practices still use this, we only employ it selectively when diagnostically necessary. The reason is that there is limited reliable evidence of its therapeutic benefit.
- Over-reliance on antibiotics for CPPS: Many centers over-prescribe antibiotics without bacterial evidence. We prioritize targeted therapy to avoid resistance and side effects.
What is the recovery process like after prostatitis treatment?
Recovery depends on the prostatitis type and treatment:
- Acute bacterial prostatitis: Symptoms often improve within days of antibiotics. Full recovery typically occurs within 2–6 weeks if the condition is treated promptly.
- Chronic bacterial prostatitis: Improvement may take weeks to months. You must be patient and adhere to your therapy protocol.
- CPPS: Recovery is gradual, with symptom relief varying from weeks to months. Lifestyle changes and ongoing therapy will improve your outcome.
Is prostatitis commonly or sometimes misdiagnosed as another condition?
Yes, prostatitis is sometimes mistaken for:
- Benign prostatic hyperplasia(BPH) and prostatitis both cause urinary issues, but BPH does not include the pain and infection of prostatitis.
- Prostate cancer: A blood test may show elevated PSA levels. A higher-than-normal PSA in prostatitis can mimic prostate cancer, but our diagnostics and attention to detail clarify the difference.
- Urinary tract infections (UTIs): Symptoms overlap, but prostatitis specifically involves the prostate.
What sets Tower Urology apart in treating prostatitis?
If you think you may have prostatitis, please know that you’re not alone, and relief is possible. Prostatitis can feel overwhelming, but with the right care, most men see improvement. We encourage you to be open about your symptoms—no detail is too small.
For chronic cases, patience is key; progress may be slow but steady. Staying proactive is essential: hydrate, manage stress, and adhere to your treatment plan. At Tower Urology, we’re here to support you every step of the way because your quality of life matters.
Tower Urology stands out with:
- Our expert team: Our board-certified urologists specialize in prostatitis, offering unmatched skill and experience.
- Cutting-edge technology: From advanced imaging to innovative therapies, we leverage the latest tools.
- Personalized care: We craft individualized plans that address the physical and emotional aspects of prostatitis.
- Comprehensive approach: Our multidisciplinary team, comprising urologists, physical therapists, and pain specialists, ensures a holistic treatment approach.
Why trust Tower Urology in Los Angeles for your prostatitis care?
Tower Urology’s board-certified urological team has been a leader in successfully treating benign prostatic hyperplasia (BPH) for over two decades, with specialists trained in all aspects of prostate health. All our professionals at Tower Urology are dedicated to providing you with expert, compassionate care. We take the time to understand you so that we can personalize your treatment plan to your specific needs.
Tower Urology’s advantage lies in our unwavering commitment to providing world-class urologic care through advanced technology, personalized treatment plans, and a patient-centered approach. With a reputation for excellence and innovation, we deliver superior outcomes that set us apart as a leader in urologic health.
Tower Urology is a proud affiliate of Cedars-Sinai Medical Center, ranked #1 in California and #2 in the nation by U.S. News & World Report. This partnership reflects our commitment to delivering the highest standard of urologic care with the best urologists in Los Angeles. Our years of experience and access to Cedars-Sinai’s world-class facilities and our exceptional, innovative, and state-of-the-art urological care make Tower Urology a leader in Southern California.
We invite you to establish care with Tower Urology.
Tower Urology is conveniently located for patients throughout Southern California and the Los Angeles area, Beverly Hills, Santa Monica, West Los Angeles, West Hollywood, Culver City, Hollywood, Venice, Marina del Rey, and Downtown Los Angeles.
Services include treatment for enlarged prostate (BPH), rezum procedure, robotic prostatectomy, and UroLift.
Prostatitis FAQs
Yes, prostatitis can affect male fertility, though the degree and mechanisms vary depending on the type and severity of the condition.
Yes, diet can affect the symptoms of prostatitis. Research and clinical experience indicate that certain foods and beverages can either aggravate or help alleviate prostatitis symptoms, especially in cases of chronic prostatitis or chronic pelvic pain syndrome.
Foods and Drinks That May Worsen Symptoms:
- Alcohol and spicy foods are commonly reported to aggravate symptoms of prostatitis.
- Caffeine (found in coffee, tea, and energy drinks) can irritate the bladder and worsen urinary symptoms.
- High-sodium foods may increase urinary tract symptoms.
- Though sensitivity varies, Gluten and red meat may contribute to inflammation in some individuals.
- Some patients report increased symptoms after consuming hot peppers, chili, and certain processed foods.
Foods That May Help Alleviate Symptoms:
- High-fiber foods (whole grains, fruits, vegetables) can help prevent constipation, which may reduce pelvic pain and discomfort.
- Healthy fats, such as those in fatty fish, nuts, and olive oil, have anti-inflammatory properties that are beneficial for prostate health.
- Cruciferous vegetables (broccoli, cauliflower, kale) and antioxidant-rich fruits (berries, tomatoes) may support prostate health and reduce inflammation.
- Herbal teas, especially green tea, may improve urine flow and decrease inflammation.
- Zinc-rich foods (nuts, seeds, shellfish, eggs) are associated with improved prostate health.
Sources
Effects of foods and beverages on the symptoms of chronic prostatitis/chronic pelvic pain syndrome
https://pubmed.ncbi.nlm.nih.gov/23978369/