What is the UroLift™ System?
The UroLift system is a minimally invasive treatment for benign prostatic hyperplasia (BPH), more commonly known as an enlarged prostate. It is also one of the few treatment options for the condition that reliably preserves sexual function.
This procedure is the most popular minimally invasive BPH procedure in the United States. It is typically performed under local anesthesia, involves no cutting, heating, or the removal of any prostate tissue, takes less than an hour, and most patients can return home the same day without a catheter.
Who is the ideal candidate for the UroLift procedure?
UroLift is a great option for men who:
- Are aged 45 years or older with symptomatic BPH
- Have a small to medium-sized prostate (generally less than 100 cc in volume)
- Prioritize a less invasive, ejaculation-sparing treatment for BPH
- Experience symptoms such as frequent urination, weak stream, difficulty starting and stopping urination, and nocturia (the need to urinate during the night)
- Have not responded well to medication or do not wish to take daily medications
- Have BPH symptoms caused primarily by the lateral lobes of the prostate with mild or no median lobe enlargement
- Have normal kidney function
- Have mild to moderate post-void residual (amount of urine left in the bladder after urinating) (less than 200 ml)
The procedure is particularly suitable for both younger, healthy men as well as older, frail men who might not be good candidates for more invasive surgical options. Men who have previously undergone prostate procedures that are no longer effective may also be candidates if there is regrowth of prostate tissue.
Who is not a good candidate for the UroLift procedure?
UroLift is not recommended for men with prostates larger than 100 cc, urinary tract infections, certain urethral conditions, urinary incontinence due to an incompetent sphincter when the sphincter doesn’t fully close (also known as stress incontinence), current gross hematuria (visible blood in urine), or known nickel, titanium, or stainless steel allergies.
How is the UroLift procedure performed?
At Tower Urology, we are equipped to perform this procedure in our office, so you are not required to make a trip to the operating room.
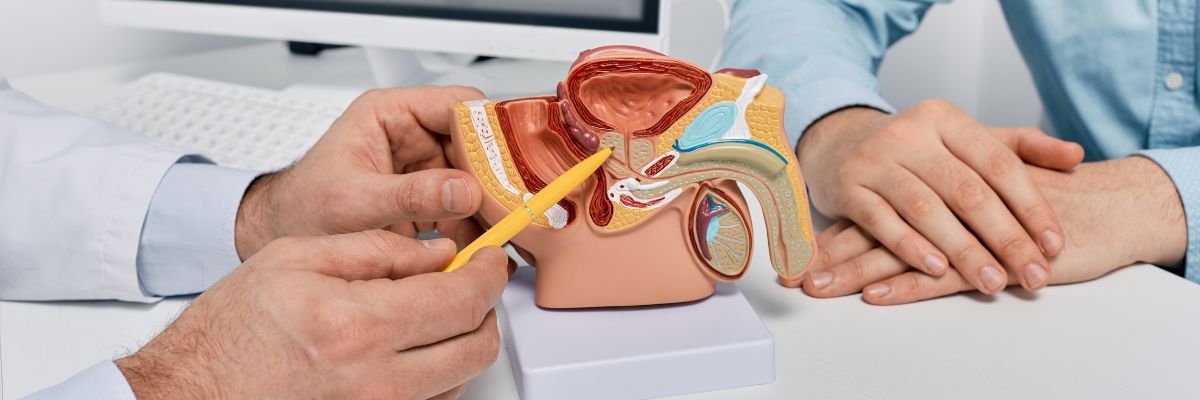
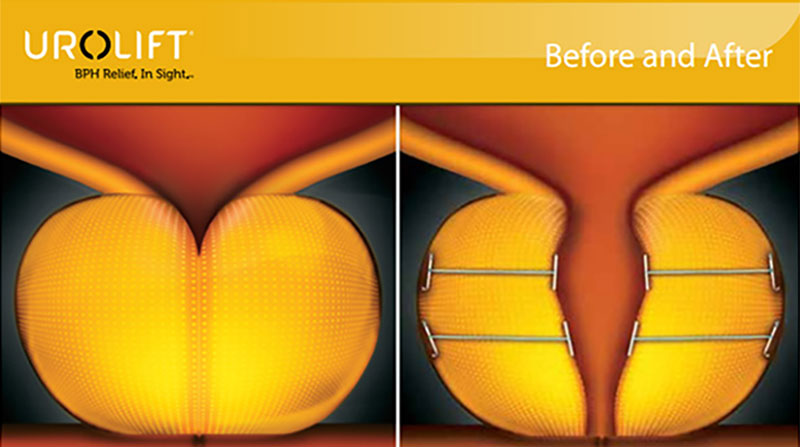
The procedure can be carried out with light sedation. First, a small camera is inserted through the urethra to access the prostate. Then, the UroLift device is used to insert the tiny implants that lift and hold the enlarged prostate tissue away from the urethra. This creates a clear path for urine to flow, relieving symptoms such as frequent urination and weak urine flow.
We usually describe it as tying curtains back.
What is the success rate of UroLift?
The UroLift procedure has high success rates, with sustained symptom improvement.
Clinical studies show that 80% of men reported being much better or very much better after the first month. A review of 10 studies, involving nearly 700 patients, revealed that almost all patients experienced overall symptom improvement, including enhanced urine flow and quality of life.
Most of Tower Urology’s patients experience fewer urinary symptoms and improved flow after undergoing this procedure. Further, only about 5-10% of men will need retreatment of their enlarged prostate in the first few years after UroLift.
Regarding long-term durability, the surgical retreatment rate (when additional procedures are needed) has varying reports:
- The official UroLift data reports a retreatment rate of approximately 13.6% over a five-year study period, or about 2-3% per year
- A more comprehensive systematic review and meta-analysis of 11 clinical studies, encompassing 2,016 patients, found a higher surgical reintervention rate of 6.0% per year, or 28.9% at 5 years.
When retreatment is needed, the most common reinterventions are transurethral resection of the prostate (TURP) (51.0%), repeat UroLift (32.7%), and UroLift explant (19.6%).
Despite these retreatment rates, UroLift maintains a very positive profile and remains a popular option due to its minimally invasive nature, preservation of sexual function, and quick recovery time compared to more invasive surgical options.
Furthermore, clinical studies have shown that the UroLift procedure does not cause new, sustained instances of sexual dysfunction.
What are the risk factors of the UroLift procedure?
As the UroLift clips are placed into the prostate, there is a risk of heavy bleeding after the procedure, and this may require the placement of a Foley catheter (a type of urinary catheter). However, if more severe, intervention under general anesthesia in the operating room may be required to stop the bleeding using a small camera inserted through the urethra.
What is recovery after UroLift like?
Recovery from UroLift is generally quick with minimal restrictions. Patients typically return home on the day of the procedure and can resume normal daily activities, except for strenuous activities, within one to two days. It is normal to experience a brief worsening of bladder irritation symptoms (burning, frequency, urgency) and blood in the urine after the procedure, but these symptoms should improve within one to two weeks.
Are there other treatment options to consider when treating benign prostatic hyperplasia?
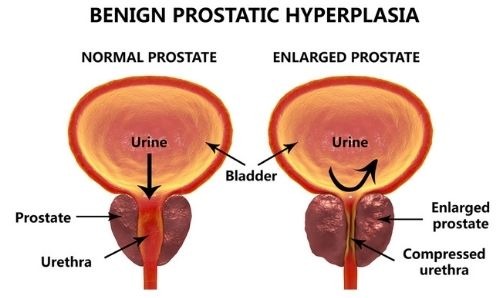
Yes, there are a multitude of options to treat benign prostatic hyperplasia (BPH). The options that are available to you depend first on the size and anatomy of your prostate. This is usually determined using imaging techniques, such as ultrasound, to examine the prostate and/or a cystoscopy, where a thin, flexible tube is inserted into the urethra to allow for internal visual examination.
Then, based on your priorities, our urologist can suggest a BPH procedure that best suits you.
A few final thoughts on the UroLift procedure
While UroLift is not the most definitive option for treating an enlarged prostate, it is an excellent option for men with a small to moderate enlarged prostate who want a less invasive approach with minimal recovery.
One thing our board-certified urologists emphasize to our patients regarding the treatment of BPH is that ejaculation-sparing refers specifically to the ability to ejaculate and not particularly to the literal ejaculate. Ejaculation-sparing aims to preserve erectile function, sensation, and orgasm as much as possible, but individual patients should be aware that they may experience modifications.
Tower Urology has the best urologists with the most experience in Los Angeles, California
The advantage of Tower Urology lies in our unwavering commitment to providing world-class urologic care through advanced technology, personalized treatment plans, and a patient-centered approach. With a reputation for excellence and innovation, we deliver superior outcomes that distinguish us as leaders in urologic health.
Tower Urology is a proud affiliate of Cedars-Sinai Medical Center, ranked #1 in California and #2 nationwide by U.S. News & World Report. This partnership reflects our dedication to delivering the highest standard of urologic care alongside the best urologists in Los Angeles.
Our years of experience and access to Cedars-Sinai’s world-class facilities ensure that our exceptional and innovative urological care positions Tower Urology as a leader in Southern California.
We invite you to establish a care plan with Tower Urology.
Tower Urology’s healthcare professionals are conveniently located for patients throughout Southern California and the Los Angeles area, including Beverly Hills, Santa Monica, West Los Angeles, West Hollywood, Culver City, Hollywood, Venice, Marina del Rey, the San Fernando Valley, Burbank, and Downtown Los Angeles.
Our men’s health specialists treat all urological conditions, including prostate cancer, bladder cancer, testicular cancer, kidney cancer, kidney stones, and male infertility, to name a few.
UroLift FAQs
Rezum and UroLift are two leading minimally invasive treatments for benign prostatic hyperplasia (BPH), each with distinct advantages and characteristics.
Treatment differences
Rezum uses water vapor therapy (convective water vapor ablation) to reduce the size of the prostate. During the procedure, steam is delivered directly into the prostate tissue, shrinking it over time as the body absorbs the treated cells. This thermal therapy effectively destroys prostate tissue using heat energy.
In contrast, the UroLift procedure uses a mechanical approach, inserting tiny implants to lift and hold the enlarged prostate tissue away from the urethra without cutting, heating, or removing prostate tissue. Compressing the prostate rather than destroying tissue creates a clear path for urine flow.
Effectiveness comparison (UroLift vs. Rezum)
Symptom relief
- Both treatments significantly improve the International Prostate Symptom Score (IPSS) at three months (approximately 50% reduction).
- Rezum achieved greater long-term symptom improvement compared to UroLift at 24 and 36 months.
- UroLift provides more immediate symptom relief, while Rezum improvements take about one month, as destroyed tissue needs to be resorbed.
Flow rate improvement
- Rezum showed greater improvement in peak urinary flow rate (Qmax) at three months (6.4 vs. 4.29 ml/sec)
- By 12–36 months, both treatments showed similar flow rate improvements.
Sexual function
- Neither procedure causes new-onset erectile dysfunction.
- UroLift demonstrated better preservation of ejaculatory function compared to Rezum.
- UroLift is the only leading BPH procedure not shown to cause new onset or sustained erectile or ejaculatory dysfunction.
Recovery and side effects
UroLift:
- Faster recovery (about one week)
- Higher rate of being catheter-free on day three (93% vs. 45% for Rezum)
- More frequent clot retention
Rezum:
- Longer recovery period (two to four weeks)
- Higher rates of urinary retention, hematuria, and dysuria in the short-term
Durability and retreatment
Retreatment rates:
- Rezum: 4.4% surgical retreatment rate at four to five years
- UroLift: 13.6% surgical retreatment rate at five years in the original studies
- A more comprehensive meta-analysis estimated UroLift’s five-year surgical retreatment rate at 28.9%
Ideal candidates
UroLift is ideal for:
- Men with mild to moderate prostate enlargement
- Those seeking immediate symptom relief
- Patients prioritizing sexual function preservation
Rezum is better suited for:
- Men with larger prostates or more severe symptoms
- Those who can tolerate a longer recovery period for potentially more durable results
- Patients with median lobe enlargement
Both procedures offer significant advantages over traditional surgical options, particularly in preserving sexual function and providing effective symptom relief with minimal invasiveness and faster recovery.
Yes they do! You can visit the Urolift Patient Portal at https://uroliftpatienteducationportal.onfulfillment.com.
Sources
Boston Scientific publication summary on UroLift surgical reintervention rates
https://www.bostonscientific.com/content/dam/bostonscientific/uro-wh/portfolio-group/health-conditions/Enlarged%20Prostate/rezum/PDF/URO-841302-AB-UroLift-meta-analysis-publication-summary.pdf
FDA documentation on the NeoTract UroLift System
https://www.accessdata.fda.gov/CDRH510K/K133281.pdf
Recent advances in UroLift: A comprehensive overview
https://pmc.ncbi.nlm.nih.gov/articles/PMC9612739/
New data show early intervention with the UroLift system improves long-term BPH outcomes
https://interventionalnews.com/new-data-show-early-intervention-with-UroLift-system-improves-long-term-bph-outcomes/