What is clitoral pain(clitorodynia)?
Clitoral pain— medically known as clitorodynia —affects the most sensitive part of a woman’s body. Despite this fact, it remained relatively unstudied until very recently. Fortunately, a new generation of gynecologists and urology researchers has learned much more about its causes and risk factors. The result was the development of new surgical treatments, which promise to bring relief for up to 23% of all women with sexual dysfunction.

What is a clitoral adhesion?
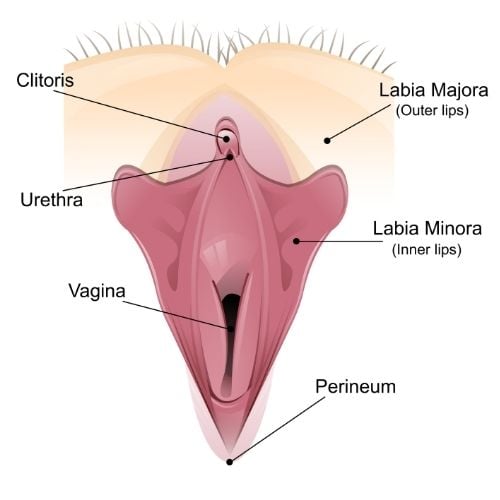
Clitoral adhesions are a condition that occurs when the clitoral hood or prepuce — the fold of skin that covers the clitoris —becomes partially stuck to the surrounding glans clitoris, the small nub of flesh right above the vulva.
Sometimes, these adhesions can surround the clitoral prepuce almost completely, forming a closed compartment or “pocket” around the clitoris. This more severe form is known as clitoral phimosis.
Often, these adhesions appear alongside keratin pearls or firm, round masses of keratinized squamous cells. Depending on their location, keratin pearls can rub against the labia, further increasing pain.
Due to a combination of cultural taboos, stigma, and their relatively “hidden location,” clitoral adhesions are often underdiagnosed. While we don’t have exact numbers on how common this condition is, some estimates point out that up to one-third of all women suffer from clitoral adhesions, making this a serious sexual health concern.
Clitoral adhesion symptoms
Clitoral adhesions can generally be diagnosed by taking a direct look at the clitoral area, as the clitoral hood will appear stuck to the clitoris. However, since this is a problematic view, the most noticeable symptoms of this condition are generally pain or soreness.
Due to the large number of nerve endings in the area, adhesions can also cause vulvar pain (vulvodynia) or be felt across the outer genitals (vestibulodynia).
Adhesions can also create:
- Redness and swelling around the hood
- Itching
- Irritation
- Pelvic pain
- Hypersensitivity or unwanted arousal (persistent genital arousal disorder)
- Pain during sexual intercourse (dyspareunia)
- Decreased sensitivity in the clitoris
- Difficulties achieving orgasm
The intensity of these symptoms often varies depending on the menstrual cycle, after sexual activity, or even during everyday activities such as biking or wearing tight clothing.
Complications of clitoral adhesions
Untreated or severe clitoral adhesions can increase the risk of a host of other problems with your gynecological or sexual functioning:
- Smegma (a buildup of a cheesy-looking substance) under the prepuce
- Frequent yeast infections
- Keratin pearls
- Problems with lubrication
- Pain when sexually aroused
- Scarring near the genital area
- Pelvic floor muscle dysfunction (when the pelvic floor muscles become weaker or uncoordinated)
What causes clitoral adhesions?
Clitoral adhesions can form due to inflammation, scarring, hormonal changes, infections, or hygiene practices. In turn, these can be influenced by:
- Chronic vulvar or bladder infections.
- Recurrent bacterial vaginosis.
- Physical trauma, whether from childbirth, surgery, or aggressive sexual activity.
- Low estrogen levels, particularly during menopause, cause thinning and dryness of the genital tissues.
- Inadequate cleaning of the genital area (from poor wiping to overusing douches or scented cleansers).
- Skin conditions affecting the genital area, such as lichen sclerosus, lichen planus, or dermatosis.
- Allergic reactions to latex condoms, spermicides, or creams.
How do we diagnose clitoral adhesions?
To diagnose this condition, your healthcare professionals at Tower Urology will perform a physical exam and ask about your symptoms and medical history.
Often, the adhesions are visible to the naked eye. However, excluding underlying skin conditions or a more serious problem may still be necessary.
If we suspect an underlying skin condition, such as lichen sclerosus or lichen planus, we may need to take a small tissue sample for further testing. Likewise, if we find any visible keratin pearls, we may perform a biopsy to rule out squamous cell carcinoma.
Treating clitoral pain and adhesions
Treatment options for clitoral adhesions focus on breaking up or removing the existing adhesions and preventing the onset of new ones.
Topical treatments for clitoral pain
For mild or new cases (or when dealing with sporadic clitoris pain during pregnancy), we generally start with topical treatments.
These include estrogen creams, which can stimulate healthy tissue and lubrication, and steroid creams, which reduce inflammation. If we believe the cause of the adhesions is hormonal, we may work alongside a gynecologist to provide oral hormone replacement therapy.
Surgical options for clitorodynia
In more advanced cases, we may need to manually separate or remove the adhesions. The most common method for clitoral adhesion surgery is known as “clitoral lysis of adhesions.” It is technically a surgery, albeit a minor one; it can be performed in-office under local anesthesia.
During a lysis procedure, a urologist will use a special type of fine forceps to separate the clitoris from its hood — no cutting or stitching is needed. For more severe cases of phimosis (when over 75% of the clitoris is covered by the hood), a more complex “dorsal slit” may be necessary.
This requires making a very fine incision right above the clitoris to open up the “compartment” or pocket that has closed around it.
Struggling with clitoris pain and clitoral adhesions? Let Tower Urology help!
Clitoral adhesions can affect a woman’s physical health, psychological well-being, and sexual pleasure simultaneously. Prompt and compassionate treatment will have a profound, positive impact on your quality of life and overall wellness.
It’s important to establish care with a healthcare provider who will continue to work with you to find the solution that is right for you individually. Fortunately, the urologists at Tower Urology are experts in treating this condition and are always willing to help. Our approach is personal—we treat patients, not just pathology.
Tower Urology is a proud affiliate of Cedars-Sinai Medical Center, ranked #1 in California and #2 nationwide by U.S. News & World Report. This partnership reflects our dedication to delivering the highest standard of urologic care alongside the best urologists in Los Angeles. Our years of experience and access to Cedars-Sinai’s world-class facilities ensure that our exceptional and innovative urological care positions Tower Urology as a leader in Southern California.
We invite you to establish care with Tower Urology.
Tower Urology is conveniently located for patients throughout Southern California and the Los Angeles area, including Beverly Hills, Santa Monica, West Los Angeles, West Hollywood, Culver City, Hollywood, Venice, Marina del Rey, and Downtown Los Angeles.
Our services include treatment for vaginal dryness, painful sex, low libido, and anorgasmia.
Clitoris pain and clitoral adhesions FAQs
The pain may fluctuate throughout the day and can affect the entire genital region or pelvic area. Some people experience persistent symptoms, while others have intermittent pain.
If you experience these symptoms, seeking medical evaluation is important, as most causes are treatable with appropriate medical intervention.
Clitoral nerve pain and damage can present with several distinct sensations:
- Sharp or stabbing pains.
- Burning sensations.
- Tingling or pins-and-needles feeling.
- Raw or irritated feeling.
- Throbbing or aching.
Clitoral adhesions are more common among women with the following conditions:
- Chronic inflammation or auto-immune disorders.
- Lichen sclerosus.
- Low levels of free testosterone.
- Diabetes mellitus.
In addition, women who have suffered blunt trauma to the genital area or tears during childbirth are also more likely to develop them.
Keeping the area clean and avoiding irritants is essential to prevent recurring problems. If you’re experiencing pain, we can discuss options like over-the-counter pain relievers or topical anesthetics to help you manage it.
No, lichen sclerosus does not spread between people. It is not contagious and cannot be transmitted through sexual contact, skin-to-skin contact, or any other form of close contact.
No, vulvar lichen sclerosus (VLS) has no cure, but proper treatment can effectively manage the condition.
Sources
Reduced Satisfaction and Increased Recurrence after Lysis Procedure for Clitoral Adhesions in Patients with Persistent Genital Arousal Disorder
https://www.sciencedirect.com/science/article/abs/pii/S1743609522013613
A Retrospective Case Series on Patient Satisfaction and Efficacy of Non-Surgical Lysis of Clitoral Adhesions
https://www.sciencedirect.com/science/article/pii/S1743609522014990
Surgical Techniques: Dorsal Slit Surgery for Clitoris Phimosis
https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1743-6109.2008.01019.x
































































