What is pelvic organ prolapse?
Pelvic organ prolapse is a condition where the pelvic organs, such as the bladder, uterus, or rectum, descend or bulge into the vaginal canal due to weakened pelvic floor muscles and connective tissue. It’s more common than many realize, as studies suggest that up to 50% of women who have had children may experience some form of pelvic floor disorder in their lifetime.
What are the symptoms of pelvic organ prolapse?
Potential symptoms of pelvic organ prolapse can include:
- Pelvic pain
- Lower back pain
- Feeling heaviness in the pelvic area
- Sensation of a vaginal bulge
- Difficulty urinating, urinary incontinence, stress incontinence, and problems defecating
- Visible tissue protruding through the vagina
- If you still have a uterus, prolapse can even obstruct your kidneys

What are the most common causes of pelvic organ prolapse?
The main cause of pelvic organ prolapse is the weakening of the pelvic floor muscles and ligaments, often due to pregnancy, childbirth, or aging. Pelvic floor muscles can become stretched or damaged during childbirth, especially with vaginal deliveries.
As women age and experience hormonal changes, particularly after menopause, loss of estrogen can further weaken these structures. Other contributing factors include obesity, chronic constipation, heavy lifting, chronic coughing, and a family history of prolapse.
What are the risk factors of pelvic organ prolapse?
Numerous factors can increase the likelihood of developing pelvic organ prolapse. These include:
- Having had multiple vaginal deliveries or given birth to a larger baby (or babies) is a significant risk factor.
- Age, particularly after menopause, is another major factor, as the pelvic floor tends to weaken over time.
- Obesity, which increases pressure on the pelvic region
- Chronic health conditions like a persistent cough (from smoking or asthma) or constipation can put additional strain on the pelvic muscles.
What are the complications of pelvic organ prolapse?
Pelvic organ prolapse can be uncomfortable and affect your quality of life. Other than urinary and fecal incontinence, some of the different possible complications of a prolapse are:
- Infection. If the prolapse prevents you from peeing, your pee could back up into your urinary tract or kidneys, causing urinary tract infections (UTIs) or kidney infections.
- Kidney damage. In severe cases, chronic infection and urine obstruction could cause kidney damage.
- Emotional distress. A prolapse can significantly disrupt your everyday life and negatively impact your emotional well-being.
What are the different types of pelvic organ prolapse?
There are several types of pelvic organ prolapse, each affecting different organs in the pelvic region.
Anterior wall prolapse
Anterior prolapse occurs when the bladder drops from its normal position and bulges into the vaginal wall and falls into three types:
- Cystocele: This is the most common type of prolapse and occurs when the bladder drops into the front wall of the vagina. It’s also called a “dropped bladder.”
- Urethrocele: This is when the urethra (the tube that carries urine from the bladder) protrudes into the vagina.
- Cystourethrocele: This condition combines cystocele and urethrocele when both the bladder and urethra prolapse.
Posterior prolapse
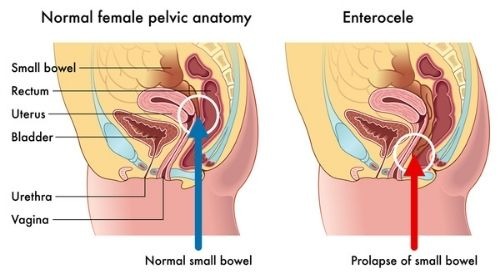
Posterior prolapse is when the wall of tissue between the rectum and the vagina weakens, causing the rectum to bulge into the vagina. There are two types of posterior prolapse:
- Rectocele: This occurs when the rectum bulges into the back wall of the vagina causing difficulties with bowel movements.
- Enterocele: This is when the small intestine prolapses into the upper part of the vagina.
Apical prolapse
Apical prolapse is when the top of the vagina or the uterus drops down due to weakened support structures in the pelvis. There are also two types of apical prolapse:
- Uterine prolapse: This is when the uterus descends into the vagina. In the most severe cases, it may protrude outside the vaginal opening.
- Vaginal vault prolapse: This occurs in women who have had a hysterectomy when the top of the vagina loses support and drops down.
Other types of pelvic organ prolapse
- Vaginal prolapse: This is when the vagina itself droops and may protrude from the body.
- Perineal descent: This is a condition where the perineum (the area between the vagina and anus) sinks below its normal position.
How do Tower Urology’s doctors determine the severity of pelvic organ prolapse?
At Tower Urology, we use a system to classify the severity of prolapse where we measure how far pelvic organs, like the uterus or bladder, have descended into or outside the vaginal canal. The most common staging system is the Pelvic Organ Prolapse Quantification (POP-Q), which divides prolapse into four stages:
Stage 1: The organs have slightly dropped but remain more than 1 cm above the vaginal opening.
Stage 2: The organs have descended to or near the vaginal opening (within 1 cm above or below).
Stage 3: The organs protrude more than 1 cm outside the vaginal opening but not entirely.
Stage 4: Complete eversion, where the organs are entirely outside the vaginal canal.
This staging system helps guide treatment decisions based on the extent of the prolapse.
What are the treatment options for pelvic organ prolapse?

Treatment depends on the severity of the condition and the symptoms.
Treatments for mild pelvic organ prolapse
In milder cases, nonsurgical treatments for pelvic organ prolapse include lifestyle modifications, such as maintaining a healthy weight, engaging in pelvic floor exercises (also known as Kegel exercises), and avoiding heavy lifting, all of which can help strengthen the pelvic muscles and prevent further prolapse. Additionally, there is a removable, silicone device called a vaginal pessary that your urologist can insert into your vagina to hold a sagging organ in place.
Treatments for more severe cases of pelvic organ prolapse
In more severe cases, quality-of-life therapies can range from the use of a vaginal pessary to help support the organs to surgical options. Any surgery is individually tailored to the severity and location of the prolapse you are experiencing, as well as other considerations, like whether you have a uterus and if you’ve had previous abdominal surgeries.
Surgical treatments for pelvic organ prolapse
Surgery for pelvic organ prolapse can be performed from a vaginal approach or by an abdominal approach. At Tower Urology, we are very experienced in both methods and will discuss the best fit for you during your consultation.
If it is determined that the abdominal approach is the right surgery for you, then we will perform it robotically, either using:
- Five incisions (which are all smaller than 1 cm) across the abdomen with the da Vinci Xi robot or
- A single two-inch incision using our Single-Port robot.
As expected, our surgeons are fully trained and extraordinarily experienced with both technologies.
Recovery after pelvic organ prolapse surgery
Regardless of the surgical approach that is deemed best for you by your urologist, recovery from pelvic organ prolapse surgery typically takes between four to eight weeks. During the recovery, you may experience mild discomfort and some fatigue, and some activities, such as heavy lifting, strenuous exercise, and sexual intercourse, may be restricted.
Most of our patients resume light activities within a few days of surgery. However, it is critically important to follow post-operative care instructions and attend follow-up appointments to help ensure complete healing and the best possible outcome.
Why Tower Urology is your best choice for pelvic organ prolapse care in Los Angeles
Tower Urology’s board-certified urological team has been a leader in effectively treating women’s healthcare for over two decades, with specialists trained in all aspects of women’s health.
The advantage of Tower Urology lies in our unwavering commitment to providing world-class urologic care through advanced technology, personalized treatment plans, and a patient-centered approach. With a reputation for excellence and innovation, we deliver superior outcomes that distinguish us as leaders in urologic health.
Tower Urology is a proud affiliate of Cedars-Sinai Medical Center, ranked #1 in California and #2 nationwide by U.S. News & World Report. This partnership reflects our dedication to delivering the highest standard of urologic care alongside the best urologists in Los Angeles. Our years of experience and access to Cedars-Sinai’s world-class facilities ensure that our exceptional and innovative urological care positions Tower Urology as a leader in Southern California.
We invite you to establish care with Tower Urology. Please make an appointment online or call us at (310) 854-9898.
Tower Urology is conveniently located for patients throughout Southern California and the Los Angeles area, including Beverly Hills, Santa Monica, West Los Angeles, West Hollywood, Culver City, Hollywood, Venice, Marina del Rey, and Downtown Los Angeles.
Our services include treatment for pelvic organ prolapse, menopause/hormone management, chronic pelvic pain syndrome in women, shockwave therapy for pelvic pain, interstitial cystitis, lichen sclerosis and planus, urethral diverticulum, urethral stricture disease, urinary fistulas, and vaginal mesh complications.
Sources
Pelvic Organ Prolapse | Cleveland Clinic
https://my.clevelandclinic.org/health/diseases/24046-pelvic-organ-prolapse
Pelvic Organ Prolapse | The Lancet
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(07)60462-0/abstract
Pelvic Organ Prolapse-A physiotherapy guide for women
https://thepogp.co.uk/resources/9/pelvic_organ_prolapse_a_physiotherapy_guide_for_women/